Abbreviated breast MRI could be a viable alternative for population-wide screening if combined with dedicated MRI systems optimized for breast imaging and ones that ensure fast patient throughput, according to Dr. Christiane Kuhl.
Kuhl, the clinical director for diagnostic and interventional radiology at Aachen University Hospital in Germany, has written a commentary in the October issue of the British Journal of Radiology that summarizes the current situation for abbreviated breast MRI and presents the EA1141 trial, which closed to accrual a year earlier than anticipated, and is designed to investigate the utility of the modality for screening average-risk women with dense breast tissue (BJR, October 2018, Vol. 91:1090, p. 20170441).
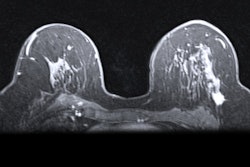
 A bilateral digital mammogram (ACR category C breast, BI-RADS 1) of a 53-year-old patient with grade 3 no special type breast cancer in the right breast. All images courtesy of Dr. Christiane Kuhl.
A bilateral digital mammogram (ACR category C breast, BI-RADS 1) of a 53-year-old patient with grade 3 no special type breast cancer in the right breast. All images courtesy of Dr. Christiane Kuhl."The promising and concordant results of several single-center studies on the utility of abbreviated breast MRI, together with the urge to find adequate supplemental breast cancer screening methods in view of the breast density legislation in the U.S., have prompted the proposal of a multicenter study that investigates the utility of a low-cost, abbreviated breast MRI as a supplemental screening test for females with dense breast tissue," she wrote.
Why breast MRI?
Mammography is a mainstay of breast cancer screening, but criticisms include how the modality overdiagnoses biologically irrelevant cancer and underdiagnoses biologically important cancer, as evidenced by continued breast cancer deaths, according to Kuhl.
"Breast MRI has repeatedly been shown to represent the most sensitive imaging method for diagnosing breast cancer regardless of stage (ductal carcinoma in situ [DCIS] or invasive) or type, and regardless of radiographic breast density," she noted. "The major advantage of MRI, however, is the fact that it improves detection of biologically relevant cancers, i.e. cancers with active angiogenic activity."
 Same patient as above. An abbreviated breast MRI (MIP image).
Same patient as above. An abbreviated breast MRI (MIP image).Physicians often recommend women at high risk of breast cancer to undergo breast MRI, but increasing evidence suggests it could be equally useful in women at average risk -- the additional cancer detection rate in a 2017 study was 15.5 per 1,000 (Radiology, May 2017, Vol. 283:2, pp. 361-370).
"Most importantly, the interval cancer rate of females undergoing MRI screening was reduced to zero," she wrote. "The more or less complete absence of interval cancers observed with MRI screening of females at average or even at increased risk of breast cancer suggests that interval cancers do not, or do not mostly, develop in between screening rounds, but are present, yet missed by current screening methods, i.e., mammography. In other words: Screening MRI detects cancers which, if MRI had not been done, would have progressed to become the more advanced interval cancers observed in females participating in usual mammographic screening."
What are the barriers to widespread breast MRI adoption? Cost, limited availability, and its false positive rate, to name a few. However, those are all obstacles that may be overcome. An abbreviated breast MRI protocol can reduce cost, and time, Kuhl believes.
 Dr. Christiane Kuhl.
Dr. Christiane Kuhl.The protocol acquires only one precontrast and one postcontrast T1-weighted image set and uses maximum intensity projections (MIP) to fuse the first postcontrast subtracted images into one single high-contrast image. Reading time was less than 3 seconds for interpreting a MIP and shorter than 30 seconds for interpreting the complete study in cases in which there was significant enhancement on the MIPs. The values are competitive with batch reading of screening mammograms and are substantially shorter than the time it takes to review tomosynthesis images.
"The specific advantage of abbreviated breast MRI is that establishing absence of breast cancer -- in other words, reviewing a negative MIP image -- is a simple task that is done within time that is counted in seconds," she wrote. "This is explainable by the fact that MIPs are high-contrast images, whereas with mammographic or tomosynthesis screening, radiologists need to meticulously search low-contrast images for subtle signs of breast cancer."
Plus, the abbreviated protocol achieves the same cancer detection rate of 18.2 per 1,000 and the same sensitivity as that achieved with the full multiparametric protocol. Several groups other than Kuhl's replicated the results, which has prompted a multicenter study that investigates low-cost, abbreviated breast MRI as a supplemental screening test for females with dense breast tissue.
New breast MRI trial
The EA1141 study, Comparison of Abbreviated Breast MRI and Digital Breast Tomosynthesis in Breast Cancer Screening in Women with Dense Breasts, is sponsored by the U.S. Eastern Cooperative Oncology Group and the American College of Radiology Imaging Network. Asymptomatic women ages 40 to 75 with dense breast tissue, defined as mammographic density categories C and D, and without breast cancer-related risk factors, will undergo digital breast tomosynthesis (DBT) and abbreviated breast MRI in randomized order for two consecutive years.
The women will then return to regular mammographic screening and be followed for another three years. The metric will be the cancer detection rate achieved by DBT versus abbreviated breast MRI in the same women in the first (prevalence) and second (incidence) screening round. Secondary objectives are to compare the positive predictive values and the type of cancers found by the two competing imaging methods.
The researchers will investigate the biological detection profiles genomic profiling studies of screen-detected cancers. They will also look at patient-reported quality of life, as well as patients' willingness to return for repeat MRI or DBT after the first study screening round. The researchers expect a sample size of 1,450 women will provide 90% power to compare the diagnostic yield regarding invasive cancer detection rates of DBT versus MRI. Accrual for the trial closed one year earlier than planned -- women were very willing to participate. Results are expected for end of this year.
Abbreviated MRI will be used as a supplemental screening tool to DBT in the EA1141 study, but future studies will examine abbreviated breast MRI as a standalone breast cancer screening method. Looking at MRI alone will also address overdiagnosis, according to Kuhl. In mammography screening, overdiagnosis is driven by detection of low- or intermediate-grade DCIS by detecting microcalcifications. MRI cannot detect microcalcifications and, thus, may remain negative in women with low-grade DCIS.
"Therefore, using MRI alone as an imaging method can be expected to help avoid diagnosis of such low-grade disease," she wrote. "Therefore, there is a reason to assume that screening by MRI alone could be useful not only to avoid underdiagnosis of biologically important cancer, but also to avoid overdiagnosis of unimportant disease."
Only time will tell.