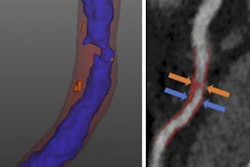
Patients with chest pain who underwent coronary CT angiography (CCTA) with standard care had a markedly lower rate of myocardial infarction or death from coronary artery disease than those who only received standard care in a new study, published on August 25 in the New England Journal of Medicine.
In a follow-up study of the Scottish Computed Tomography of the Heart (SCOT-HEART) trial, researchers from various institutions in the U.K. and Ireland examined the five-year outcomes of more than 4,000 patients whom clinicians had referred for chest pain assessment at one of 12 cardiology centers. CCTA in addition to standard care was associated with a 41% lower subsequent risk of nonfatal myocardial infarction or death from coronary artery disease than standard care alone (NEJM, August 25, 2018).
"The use of [CCTA] resulted in more correct diagnoses of coronary heart disease than standard care alone, which, in turn, led to the use of appropriate therapies, and this change in management resulted in fewer clinical events," wrote first author Dr. David Newby, from the University of Edinburgh, and colleagues.
Long-term outcomes of CCTA
Several major studies, such as SCOT-HEART and the Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE), have shown that CCTA can improve the diagnosis of obstructive coronary artery disease as well as reduce adverse event rates, compared with standard care.
Despite the apparent advantages of using CCTA to evaluate chest pain, various groups have been wary of the test due to its potential to increase hospital length of stay, radiation exposure, and related costs. Indeed, an analysis of data from the Rule Out Myocardial Ischemia/Infarction Using Computer-Assisted Tomography (ROMICAT) II trial revealed that CCTA did not reduce major adverse cardiac events more effectively than clinical evaluation alone -- although the scope of this trial was limited by its short duration of only 28 days.
One way to address such concerns could be to demonstrate the positive effect of CCTA on long-term clinical outcomes. To that end, the investigators in the present study examined data from the 4,146 patients of the SCOT-HEART trial. The median duration of patient observation for this cohort was 4.8 years, compared with 20 months in the initial trial.
Newby and colleagues randomly assigned half of the patients (2,073) to undergo a CCTA exam along with routine clinical evaluation (i.e., exercise electrocardiography or stress imaging) and half to receive only routine evaluation. The randomization method balanced patient characteristics such as age, sex, and history of heart disease. The researchers also prompted the physicians caring for the patients to manage each condition using all available information, including results from the CCTA exams.
Lower rate of heart attack, death
After following the participants of the SCOT-HEART trial for five years, the researchers found that the CCTA group had fewer nonfatal myocardial infarctions or death due to coronary artery disease than the standard-care group by a statistically significant degree (p = 0.004).
Overall, an initial diagnostic strategy that incorporated CCTA in addition to standard care had a considerably lower rate of heart attack or death from coronary artery disease. To be specific, 48 patients in the CCTA group had a heart attack or died, compared with 81 in the standard-care group.
| SCOT-HEART trial comparing standard care vs. CCTA + standard care | ||
| Outcome | Standard care | Standard care + CCTA |
| Death from coronary heart disease or nonfatal heart attack | 3.9% | 2.3% |
| Invasive angiography | 24.2% | 23.7% |
| Revascularization | 12.9% | 13.5% |
| Antianginal therapies | 10.7% | 13.2% |
| Preventive therapies | 14.7% | 19.4% |
This decrease in the risk of heart attack or death came without a significant increase in the rate of invasive procedures, namely, invasive coronary angiography and coronary revascularization. Instead, the CCTA group received a slightly higher number of less invasive antianginal and preventive therapies (such as aspirin and a statin).
"Beyond 12 months, rates of invasive coronary angiography and coronary revascularization were higher in the standard-care group than in the CTA group," the authors wrote. "This would be consistent with both the emergence of unrecognized disease and nonfatal myocardial infarction in the standard-care group and the reduction in disease progression in the CTA group owing to the implementation of lifestyle modifications and preventive therapies."
The authors acknowledged several limitations to their study, including an inherent bias in the trial design favoring CCTA (because clinical diagnoses relied on knowledge of the assigned groups) and a lack of information on the lifestyle alterations that patients in the CCTA group made after undergoing the exam.
A different perspective
Newby and colleagues suggested that the lower incidence of heart attacks and death in the CCTA group, compared with the standard-care group in the SCOT-HEART trial, likely occurred as a result of changes in medical management after CCTA testing, including a more appropriate use of preventive therapies.
However, the differences in medical management between the groups were modest and do not seem to be sufficient to explain the much lower rate of heart attacks and death in the CCTA group, Dr. Udo Hoffmann of Massachusetts General Hospital and Dr. James Udelson of Tufts Medical Center wrote in an accompanying editorial. Both Hoffmann and Udelson were authors of PROMISE.
Regarding clinical outcome, the results of the SCOT-HEART trial stand in contrast to those of PROMISE, which showed no statistically significant difference in outcomes between CCTA and standard care over the course of the trial's two-year follow-up period.
A standout distinction between the two trials was the type of tests physicians used for standard care, Hoffmann and Udelson noted. Whereas the routine clinical strategy for the SCOT-HEART trial primarily involved exercise electrocardiographic testing, the predominant standard-care option in the PROMISE trial was nuclear or echocardiographic stress imaging.
It is possible, then, that the reduction in heart attack and death rates for patients who underwent CCTA compared with those who underwent electrocardiography may not necessarily apply when stress imaging is used as standard of care, they continued. Further supporting this idea, aspirin use increased for the CCTA group but not for the electrocardiography group in SCOT-HEART, whereas aspirin use increased after initial testing for both groups in PROMISE.
"The more general message from these trials is that the information provided by a diagnostic test can resonate therapeutically beyond making a correct diagnosis of coronary artery disease and that clinicians should aggressively pursue preventive measures to achieve the best outcomes possible while minimizing daily symptoms," they wrote.