Researchers from Germany have developed software that uses ultrasound, MRI, or CT scans of the heart to produce virtual 3D models depicting different stages of heartbeat, according to a presentation at the recent Computer Assisted Radiology and Surgery (CARS) 2018 international congress in Berlin.
The interdisciplinary team of experts, led by Anja Hennemuth, PhD, from the Fraunhofer Institute for Medical Image Computing (MEVIS) in Bremen, used these 3D heart models to simulate different variations of minimally invasive heart valve procedures for correcting heart valve insufficiency. The simulations enabled surgeons to identify the most effective technique for individual cases.
"At this time, we are validating the therapy simulation through comparison with the postsurgical data of treated patients," she told AuntMinnieEurope.com. "Hopefully, the support [the 3D models can provide] will lead to more objective decision-making and improve overall treatment quality."
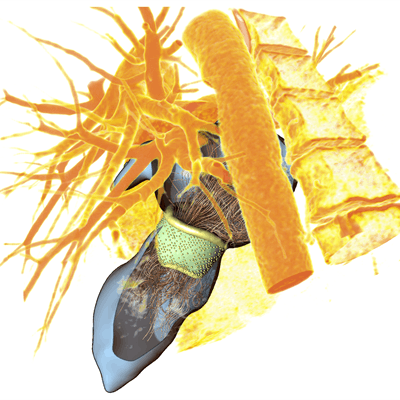
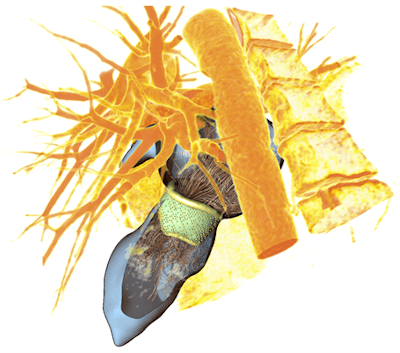 3D heart valve model with corresponding blood flow simulation. Image courtesy of Anja Hennemuth, PhD.
3D heart valve model with corresponding blood flow simulation. Image courtesy of Anja Hennemuth, PhD.Reducing leakage
Minimally invasive heart valve repair has steadily grown in popularity in Europe, with approximately 7,000 mitral valve interventions performed per year in Germany alone, Hennemuth said. Mitral valve repair has become the preferred surgical treatment over valve replacement due to its association with improved long-term outcomes. The success of this procedure relies heavily on the extent to which medical imaging reveals the mechanistic cause of valve failure in patients.
"In current practice, mitral valve repair success rates are a mean of 67% -- about 48% among less experienced surgeons and 77% among experts," she said. "These [rates] demonstrate the continued need for better decision-making support."
Responding to this need, Hennemuth and colleagues developed computer software that could facilitate the preoperative visualization of heart valves through virtual 3D models. First, they acquired ultrasound scans of the heart in different phases of heartbeat, segmented the scans, and defined key anatomical landmarks. Then they entered these edited scans into their software to generate a dynamic 3D heart model, or "heuristic geometric model," that highlighted the heart valve deformation during different phases of heartbeat.
Furthermore, the software was able to simulate mitral valve repair on these 3D heart models by virtually sewing a surgical ring around the heart valve and quantifying the amount of blood that could possibly leak back into the atrium. Thus, the software could potentially help clinicians determine the ideal type and course of surgical treatment by estimating the chances of success for each one.
The researchers are currently validating the prototype software and comparing its simulation results to real patient outcome information. They hope to implement the new method into actual surgery within the next few years and eventually apply the technique to a wide range of heart procedures.
Navigating vessels
At CARS 2018, the group also discussed a new technique using their software to guide catheters through blood vessels. Generally, navigating a catheter tip all the way to the heart involves the repeated administration of a contrast agent during x-ray fluoroscopy, which requires exposing patients to radiation multiple times.
A potentially safer alternative, the team's "shape-sensing" method reduces the need for radiation by placing sensors onto the catheter that are able to capture the way the catheter bends and turns as it travels through blood vessels. Once clinicians enter the data into the software, it combines the newly input data with prior medical images to display a detailed model of the vessel network and finally calculate the precise location of the catheter tip.
This could simplify vessel navigation and drastically diminish the burden of other, more costly imaging techniques, according to the researchers.
"So far, the results have been very good and the surgeons are satisfied," Hennemuth said. "The foundation of our success is the close interdisciplinary collaboration between Fraunhofer MEVIS, Charité, and the team of Dr. Volkmar Falk at the German Heart Center in Berlin."