By targeting certain biomarkers, conventional MRI scans can help accurately classify soft-tissue sarcoma after core needle biopsy, according to a French study presented at ECR 2018 in Vienna.
Researchers found the degree of necrosis and tumor margins on contrast-enhanced T1-weighted MR images, as well as contrast uptake in edema enhancement, contributed to the correct classification of high grade 3 tumors.
"Interestingly, they were truly reproducible in terms of agreement for necrosis, the margins, and contrast uptake in edema enhancement," said lead author Dr. Amandine Crombé from the Bergonié Institute in Bordeaux. "There is, of course, the need for a validation cohort in the prospective study."
Tumor varieties
Soft-tissue sarcoma includes a group of more than 50 different types of tumors, the prognosis and management of which strongly rely on histopathological grading. Traditionally, grading a soft-tissue sarcoma has been done through surgical specimens, with current guidelines recommending physicians perform multiple needle core biopsies after appropriate imaging assessment.
With soft-tissue sarcoma, the three main prognostic factors for the disease -- size, depth, and grading -- are based on U.S. National Cancer Institute (NCI) guidelines and French Federation Nationale des Centers de Lutte Contre le Cancer (FNCLCC) standards, which are practiced in Europe.
The FNCLCC system is based on three characteristics. One criterion is the scoring of cancer cells, with a grade of 1 as an appearance similar to normal cells and 3 as very abnormal. Certain types of sarcoma are automatically given a higher score.
In addition, there is the mitotic count, or division of cancer cells. The fewer cancer cells seen dividing indicate a lower grade of tumor. The third factor is tumor necrosis of the amount of dying tissue. A lower score suggests more living tissue.
"It has been demonstrated in several studies the three criteria are diagnostic factors for overall survival and metastatic disease-free survival, with grade 3 indicating a poor prognosis," Crombé told ECR attendees. "The grade is used to make therapeutic decisions based on risk stratification, with grade 3, or high-grade soft-tissue sarcoma when it is locally advanced, is an indication for neoadjuvant treatments."
Needle core biopsy of soft-tissue sarcomas, however, is not foolproof relative to FNCLCC histological grading because the tumors' small sample size can hinder the determination of necrosis and tumor activity.
Risky evaluation
"There is, however, a risk of underestimating the grade of the tumor due to its heterogeneity," Crombé added. "So the purpose of this study was to identify MRI features associated with high grade 3 soft-tissue sarcoma. The second step was to see how these MRI features could reclassify low grade 1 in grade 2 soft-tissue sarcoma after needle core biopsies."
Through a cancer network database, the researchers retrospectively identified 130 adult patients (median age of 60.9, range 18 to 90 years old) with soft-tissue sarcoma in their trunk wall and extremities. The patients also were available for pretreatment MRI, which would include protocol of contrast-enhanced T1- and T2-weighted imaging sequences.
Of the 130 cases, 69 (53%) patients had grade 3 sarcomas, 47 (36%) individuals had grade 2 disease, and 14 (11%) patients with low grade 1 sarcoma. Most of the sarcomas were located in the lower limbs (85 tumors, 65%) and at the trunk wall (29 tumors, 23%).
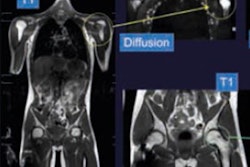
Two radiologists reviewed the MR images and evaluated the sarcomas' size, depth, and location, as well as six other factors to classify the tumors: T1 heterogeneity, T2 heterogeneity, necrosis, margins on T2-weighted images, margins on contrast-enhanced T1-weighted images, the degree of edema, and edema enhancement.
Through a multivariate analysis, the researchers discovered the three following independent predictors of true grade 3 soft-tissue sarcomas:
- Ill-defined tumor margins of greater than 10% of tumor surface on postcontrast T1-weighted imaging (odds ratio [OR] = 2.93, p = 0.026)
- Necrotic signal (OR = 2.82, p = 0.013)
- Surrounding edema enhancement (OR = 3.55, p = 0.004)
"Together these three features were seen in 34 (26%) of 130 tumors, of which 28 (82%) were high grade 3 soft-tissue sarcomas," Crombé said.
The researchers also looked at a subset of 34 patients with low grade 2 tumors and nine patients with low grade 1, both based on needle core biopsy results. Of those 43 subjects, 29 individuals (67%) were confirmed to have true low grade 1 or grade 2 tumors, while 14 cases were upgraded to true high grade 3 sarcomas.
"We can see the two of the three [factors] -- necrosis and margins on postcontrast T1-weighted imaging -- correctly reclassified more than 85% of the 14 upgraded patients," she noted.
The results need to be validated in a prospective study to see how other imaging modalities, such as PET/CT, diffusion-weighted MRI, dynamic contrast-enhanced MRI, and MR spectroscopy perform, she concluded.