Radiologists can plan and simulate vascular procedures on patient-specific and cost-effective 3D-printed stenosis models by using a new technique developed in Basel, Switzerland.
By filling in 3D-printed scaffolds with silicone rubber, researchers were able to generate replicas of stenotic vessels at a more affordable price than most other currently available methods. Their technique, introduced in a presentation at the RSNA 2017 meeting in Chicago, involves using a fused filament fabrication 3D printer and silicone molding to reproduce the 3D-printed stenosis models.
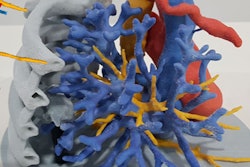
 Angiography simulator. Image courtesy of Dr. Reinhard Kaufmann.
Angiography simulator. Image courtesy of Dr. Reinhard Kaufmann."Not only will this [technique] allow residents to train on a model to become familiar with vascular procedures in a cost-effective manner, but it will also enable experienced interventional radiologists to practice and plan complicated interventions prior to the actual angiography," Dr. Philipp Brantner, co-head of University Hospital Basel's 3D Print Lab, told AuntMinnieEurope.com.
Combining technologies
As the complexity of interventional radiological procedures and economic pressure on hospital departments continue to grow, so, too, does the challenge of adequately educating and preparing residents to meet elevated standards, he said. Numerous training protocols for operations have already been established, but most of these practices rely on anatomic phantoms that are generally expensive and rarely tailored to individual patients.
A popular alternative to training with phantoms is to use 3D-printed models. The McKinsey Global Institute estimated that 3D printing would make about $550 billion U.S. or 448.1 billion euros in 2025, and ranked its potential economic impact ninth among disruptive technologies such as cloud computing and advanced robotics. Research has further shown that simulating procedures on 3D-printed models can help optimize surgical accuracy and shorten surgery times.
Hoping to take advantage of this potential boost in efficiency, Brantner and colleagues developed a technique to create low-cost 3D-printed models of stenotic vessels at the university 3D Print Lab. Producing models in-house could not only increase affordability and access to the models, but also improve patient care and outcomes, according to the group.
They first segmented CT scans of stenotic vessels and used open source 3D modeling software (3D Slicer) to design a generic stenosis model adapted for angiography simulation based on the scans. They then printed out a negative form of the design with a fused filament fabrication 3D printer. This negative form served as a scaffold for the final model, which the researchers fashioned by filling in the scaffold with clear, flexible silicone consisting of a texture that resembles vasculature.
The resulting generic vascular stenosis model allowed the researchers to simulate angiography at a much lower cost (estimated at $10 U.S. or 8.15 euros) than using typical anatomic phantoms that can cost hundreds of euros. Surgical training using the model has since been incorporated into several interventional radiology and vascular surgery courses associated with University Hospital Basel.
Following the same technique, the researchers subsequently created a different 3D-printed vasculature model based on a CT scan of the forearm, which radiographers/technologists could use to train for vascular access management. The model contains veins with diameters of up to 4 mm and can be connected to an infusion pump providing simple gravity-based vascular flow.
Uniting the image segmentation, 3D modeling, and scaffolding processes of 3D printing with silicone molding proved to be an easy and cost-effective way to develop reproducible vascular models, Brantner said. The key implications associated with this 3D printing technique are the fabrication of low-cost training models for vascular procedures, training in the early phase of resident education, and simulation on patient-specific models prior to high-risk interventions.
"In the future, we hope to create our own low-cost angiography simulator based on open-source hardware and to expand on creating not only generic stenosis, but also patient-specific and more complex vessel variants," he said.
Recently, the researchers have been updating their technique for modeling stenosis precisely that way. Whereas they previously filled a negative printout with silicone, they are now using a stereolithography 3D printer and near-transparent resin to model the vessels. A test version of the new 3D-printed stenosis model includes a generic silicone tube for access to vasculature, a small pump to provide flow, and a LCD panel for backlighting.
“While the vessel print is more costly than the silicone 3D-printed stenosis [model], it allows you to print complex vasculature, which we did not achieve with the silicone molding,” he said.