Prostate cancer remains one of the most common indications for radiotherapy, but its treatment is set to be transformed by the arrival of MRI-guided linacs in hospitals, promising improved disease control and reduced side effects.
An international collaboration of clinicians and physicists is exploring the opportunities, benefits, and challenges of MRI-guided adaptive radiotherapy of the prostate and describes the current state-of-the-art (International Journal of Radiation Oncology, Biology, and Physics, 26 October 2017). The authors include researchers from sites involved in research using the Unity MR-linac and MRIdian treatment systems from Elekta and ViewRay, respectively, the two companies with MRI-guided radiotherapy technology in clinical use.
For some time, MRI has been regarded by many in the radiation oncology community as the future of image guidance. The high soft-tissue contrast images that it provides of the patient on the treatment couch is a key advantage over conventional x-ray guided linacs. Exploiting such information to adapt plans over the course of treatment is a critical step forward, according to first author Angela Pathmanathan, a clinical fellow at the Institute of Cancer Research and the Royal Marsden Hospital in London.
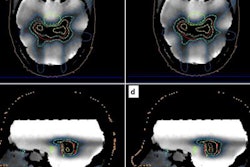
 A clinical image of a prostate produced using a steady-state TrueFISP MR sequence acquired on a ViewRay 0.35-tesla MRIdian system in 25 seconds. Reprinted from Int. J. Radiat. Oncol. Biol. Phys. doi: 10.1016/j.ijrobp.2017.10.020 © 2017, with permission from Elsevier.
A clinical image of a prostate produced using a steady-state TrueFISP MR sequence acquired on a ViewRay 0.35-tesla MRIdian system in 25 seconds. Reprinted from Int. J. Radiat. Oncol. Biol. Phys. doi: 10.1016/j.ijrobp.2017.10.020 © 2017, with permission from Elsevier."By acquiring MR images prior to each fraction, we can produce a new radiotherapy plan for that day, adjusted for any changes in anatomy," Pathmanathan explained. "With MR guidance, this can be further adjusted whilst the patient is having the radiotherapy delivered, to take into account intrafractional movement of the prostate and the 'bystander' organs-at-risk."
The next step
Online plan adaptation immediately prior to irradiation has already been demonstrated using both the ViewRay MRIdian cobalt-60 system and the Unity MR-linac. Real-time adaptive radiotherapy, while the treatment beam is on, remains a significantly greater challenge. Pathmanathan sees timing as the greatest hurdle in implementing both adaptive approaches.
"Online and real-time replanning ... must be rapid enough to still reflect the anatomy," she said. "The overall time for the patient on the bed needs to be minimized to reduce patient movement and improve comfort." Doing so requires optimization of each step in the treatment workflow, from imaging and contouring to plan optimization, along with the update of beam parameters and quality assurance.
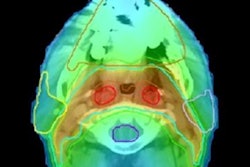
 Rapid, accurate, automated segmentation algorithms are needed to handle large volumes of images that adaptive radiotherapy requires. Echo sequences optimized to better visualize the prostate can improve segmentation accuracy. Image credit: Maria Schmidt, Royal Marsden Hospital/Institute of Cancer Research. Reprinted from Int. J. Radiat. Oncol. Biol. Phys. doi: 10.1016/j.ijrobp.2017.10.020 © 2017, with permission from Elsevier.
Rapid, accurate, automated segmentation algorithms are needed to handle large volumes of images that adaptive radiotherapy requires. Echo sequences optimized to better visualize the prostate can improve segmentation accuracy. Image credit: Maria Schmidt, Royal Marsden Hospital/Institute of Cancer Research. Reprinted from Int. J. Radiat. Oncol. Biol. Phys. doi: 10.1016/j.ijrobp.2017.10.020 © 2017, with permission from Elsevier.Using adaptive MRI-guided treatments, prostate patients could benefit from more extreme hypofractionation than is currently achievable with external beams, including, potentially, single fraction treatments. Reduced fractions cut the numbers of clinic visits for patients, increase patient throughput, and could improve clinical outcomes.
Adaptive MRI-guided radiotherapy could also improve treatments by targeting tumor subvolumes that respond poorly to treatment and carry a greater risk of recurrence. Though significant research is still needed, diffusion-weighted imaging (DWI) has been flagged by researchers as a promising approach for monitoring tumor response.
 U.K. prostate trials in the last 15 years illustrate how hypofractionation is increasingly favored. Reprinted from Int. J. Radiat. Oncol. Biol. Phys. doi: 10.1016/j.ijrobp.2017.10.020 © 2017, with permission from Elsevier.
U.K. prostate trials in the last 15 years illustrate how hypofractionation is increasingly favored. Reprinted from Int. J. Radiat. Oncol. Biol. Phys. doi: 10.1016/j.ijrobp.2017.10.020 © 2017, with permission from Elsevier.A further dramatic shift in approach is the potential elimination of CT scans from clinical workflow. Doing so eliminates geometric uncertainties resulting from the co-registration of MR and CT images and one less scan is required. However, an alternative strategy is needed to map electron density in the patient in order to calculate treatment plans.
Currently, MRCAT from Philips Healthcare is the only commercial product available, with a reported dosimetric accuracy of 0.5% compared with CT calculated dose distributions. It generates pseudo-CT scans from an mDIXON echo sequence, automatically segmenting five types of tissue using a classification algorithm and pelvic bone atlas. Voxels are assigned bulk Hounsfield units according to their classification.
Moving forward, the consortium partners are currently working on preclinical prostate studies. The first patients will be treated at consortium sites in early 2018 following a jointly written protocol, enabling data to be pooled for analysis. As a starting point, patients will receive a conventional fractionation of 60 Gy in 20 fractions to assess feasibility and adverse effects.
"Initial treatment will be with a mixed CT and MR workflow with online replanning prior to each treatment and the use of prostate motion monitoring within each fraction," Pathmanathan told medicalphysicsweb.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.