Automated breast volume scanning (ABVS) performs better than ultrasound and MRI in predicting breast cancer size for lesions smaller than 2 cm, and it is comparable for lesions of all other sizes, according to Italian researchers.
In a study of 100 women who underwent ultrasound and ABVS followed by MRI, researchers from the Institute of Diagnostic Radiology at University Hospital in Udine compared the three modalities and found ABVS is equivalent to ultrasound in predicting lesion size in some cases and approaches MRI in others.
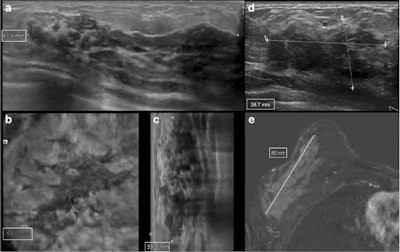 Measurements of ductal carcinoma in situ (DCIS) of the right breast in a 51-year-old woman. ABVS (a, axial plane; b, coronal reconstruction; c, sagittal reconstruction) showed an inhomogeneously hypoechoic mass with irregular margins and with the largest diameter of 67 mm. On ultrasound, (d) the same lesion had a maximum diameter of 39 mm, while on MRI (e) one of 80 mm. Histopathological size was 85 mm. All images courtesy of European Radiology.
Measurements of ductal carcinoma in situ (DCIS) of the right breast in a 51-year-old woman. ABVS (a, axial plane; b, coronal reconstruction; c, sagittal reconstruction) showed an inhomogeneously hypoechoic mass with irregular margins and with the largest diameter of 67 mm. On ultrasound, (d) the same lesion had a maximum diameter of 39 mm, while on MRI (e) one of 80 mm. Histopathological size was 85 mm. All images courtesy of European Radiology."By performing a direct comparison between MRI, ultrasound, and ABVS in predicting breast cancer size at histological examination, we confirmed the well-known superiority of MRI," wrote Dr. Rossano Girometti, researcher and staff radiologist, and colleagues (European Radiology, 10 October 2017). "However, ABVS was comparable with MRI in terms of limits of agreement with histology (i.e., the expected discrepancy in size), and was slightly more accurate than MRI in the subgroup of lesions ≤ 2 cm."
Why ABVS?
Assessing tumor size is critical in breast cancer care as size affects treatment options, such as breast-conserving surgery, and disease prognosis. MRI is king in this regard, but the modality isn't widely available, has high costs, and identifies false positives.
Conventional ultrasound is faster, cheaper, and more available but, as per usual, is operator-dependent. ABVS overcomes these limitations by providing a sonographic 3D representation of the breast tissue, with the advantage of multiplanar reformations and the capability of reviewing images retrospectively once the examination has been acquired. The device has a linear 5- to 14-MHz transducer mounted on a flexible arm with an automated one-button pressure and locking mechanism to speed and simplify the acquisition technique. The transducer scans volume slabs of up to 15.4 x 16.8 x 6 cm while acquiring 0.5-mm thick images in the transverse plane. Different preset cup sizes determined an automatic adjustment of depth, focal zone placement, overall gain, and frequency.
How does ABVS perform in cancer staging? And how does it compare with conventional ultrasound and MRI? That's precisely what Girometti and colleagues sought to discover. They compared the agreement of ABVS, ultrasound, and 1.5-tesla MRI with histological examination in defining breast cancer size and evaluated the agreement between ABVS and ultrasound in defining BI-RADS descriptors and the location of neoplastic lesions.
They retrospectively included 98 women with 100 index cancers who had undergone ultrasound (iU22, Philips Healthcare or Logiq E9, GE Healthcare) and ABVS (Acuson S2000, Siemens Healthineers), followed by 1.5-tesla MRI (Magnetom Avanto, Siemens or Magnetom Aera, Siemens). Images were interpreted by a pool of readers reporting lesion size, location, and BI-RADS features.
Of the 100 cancer cases, the researchers found 59 cases of infiltrating ductal carcinoma (IDC), seven cases of ductal carcinoma in situ (DCIS), three cases of IDC with DCIS, 10 cases of infiltrating lobular carcinoma (ILC), and 11 cases of other tumors.
In terms of how each of the modalities performed, MRI showed the highest agreement with histology with a minimal bias toward overestimation. Size measurements provided by ABVS and ultrasound were highly concordant, and they showed a minimal bias toward underestimation compared with histology. However, ABVS performed better than conventional ultrasound, as shown in the table below.
| Lesion size as measured by modality | ||||
| Ultrasound | ABVS | MRI | Histological exam |
|
| All lesions | 18.2 ± 11.2 | 18.6 ± 12.1 | 22.4 ± 11.2 | 20.6 ± 16.2 |
| Invasive tumors | 18.3 ± 11.2 | 18.5 ± 11.3 | 22.2 ± 15.8 | 20.4 ± 15.3 |
| Intraductal tumors | 15.9 ± 11.5 | 20.1 ± 21.3 | 25.0 ± 24.6 | 22.7 ± 27.6 |
| Lesions ≤ 2 cm | 12.8 ± 5.4 | 12.6 ± 4.8 | 14.6 ± 5.1 | 12.3 ± 3.9 |
| Lesions > 2 cm | 29.1 ± 11.8 | 30.8 ± 13.3 | 38.2 ± 19.8 | 37.3 ± 18.7 |
Looking at the data, the results show that the cancer size measured by MRI was between 0.63 and 1.99 times the cancer size measured on the histological examination for about 95% of cases, according to the authors.
For ABVS and ultrasound, the cancer size was between 0.79 and 1.32 times the cancer size measured on the histological examination for about 95% of cases. ABVS, in particular, though showed a discrepancy in overestimating cancer size ranging from 48% below to 73% above the histological size. Also, both ABVS and ultrasound underestimated two cases of ILC and one case DCIS, but ABVS to a lesser extent.
"In our series, ABVS provided equivalent results compared with ultrasound in identifying, characterizing, and measuring breast cancer," noted Girometti, who is a professor at the University of Udine and a member of the editorial advisory board of AuntMinnieEurope.com. "We observed excellent agreement between size measurements."
The two techniques also showed substantial to almost perfect agreement in assessing the quadrant of cancer location, as well as sonographic features, including shape, orientation, margins, and echo pattern. Similarly, the results showed no significant effect on BI-RADS assessment because the high agreement in other qualitative features translated into classifying all index lesions as suspicious with both imaging techniques, with substantial agreement in BI-RADS 4-5 categories.
"One might argue that the magnitude of the differences between ABVS and ultrasound we observed is small in absolute terms, making it difficult to suggest relevant clinical effects of using ABVS," the authors concluded. "However, subgroup analysis showed that differences versus histology were more consistently in favor of ABVS for lesions > 2 cm and intraductal tumors."
Whether the results are translatable into measurable clinical gain should be investigated in further studies, they stated. However, using ABVS will overcome operator dependency at the very least.