Women may need less frequent CT lung cancer screening than men, according to a study to be presented on 6 May at the European Lung Cancer Conference (ELCC 2017) in Geneva. The finding could enable physicians to reduce CT screening frequency (and thus exposure to radiation) in women.
The study examined 46,766 individuals undergoing CT lung cancer screening between 2000 and 2016 at Asan Medical Center in Seoul, South Korea. Close to 100 patients who were initially free of the disease were diagnosed in subsequent scans.
The researchers found the time between a lung cancer diagnosis and the last CT scan was two years longer among women versus men. At the same time, the lung cancer stage at diagnosis was higher among men, with twice as many women as men diagnosed with stage I disease.
"Our study suggests that the annual follow-up interval for CT is too frequent for women, and scans every two to three years might be suitable," said Dr. Mi-Young Kim, a radiologist at Asan Medical Center, in a statement. "By reducing the number of unnecessary CT scans, we can decrease radiation exposure and increase cost-effectiveness."
The U.S. Preventive Services Task Force (USPSTF) recommends annual screening for lung cancer with low-dose CT in adults ages 55 to 80 who have a smoking history of at least 30 pack-years and are either current smokers or have quit within 15 years. The advice is the same for both genders.
This study examined gender differences in newly developed lung cancers, calculating the optimal CT screening intervals for women and men. Over the study period, a total of 282 patients developed lung cancer, including 186 who were diagnosed at baseline screening and excluded from the study, and 96 patients, including 85 men and 11 women, who were diagnosed in follow-up CT scans.
According to the results, the average time between lung cancer being diagnosed on CT and the previous CT scan was significantly longer in women (5.6 years) compared with men (3.6 years). Yet the lung cancer stage at diagnosis was higher in men: 82% of lung cancers diagnosed in women were stage I, versus just 49% in men.
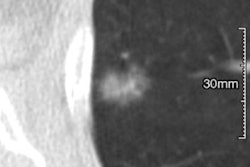
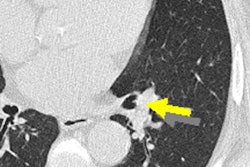
Pathological analyses showed that the most common finding in men were solid nodules (72%), while ground glass opacities (45%) were the most common finding in women, followed by squamous cell carcinoma (35%), small cell lung cancer (18%), and others (5%), the authors wrote. All female patients had adenocarcinoma.
"Because ground glass opacity nodule is the most common feature of lung cancer in women and all cases are adenocarcinoma, the growth rate of cancers might be low," Kim said in her statement. "Most female patients were nonsmokers (82%), who have a lower risk of lung cancer, while 87% of men were smokers."
And even though the study included all patients screened for lung cancer in a 17-year period, there were only 11 female patients, so additional studies will be needed to confirm the gender differences that were revealed, she added.
If these findings are confirmed in future studies, they could support less frequent screening of women and thus lower radiation exposure. However, previous studies using longer screening intervals have had mixed results, Kim said. The gender differences "may have been caused by differences in the clinical and radiological presentation of lung cancer in women and men," she said.
"The rate of nonsmoking lung cancer is different between men and women and varies among countries," Kim added. "This should be taken into account when considering a gender-based lung cancer screening policy."
In a statement, Dr. Pilar Garrido from Ramón y Cajal University Hospital in Madrid, Spain, commented that the debate about the optimal screening strategy is ongoing. and current selection criteria are based only on age and pack-years. Several studies have highlighted different lung cancer features in men and women, defining a different entity in female patients, she said.
The study, "Optimal screening interval for detection of newly developed lung cancer: Comparison of sexual difference" will be presented by Dr. Hyun Jung Koo during a poster discussion session "Epidemiology and innovations in biomarker development" on Saturday 6 May at 16:45 (CEST).