Dutch researchers are putting the finishing touches to a longitudinal study to gain more insight on vascular cognitive impairment and determine which prognostic factors could signal future cognitive decline and major vascular events, according to an article published on 17 April by the Journal of Medical Internet Research (JMIR).
The novel approach of the Utrecht-Amsterdam Clinical Features and Prognosis in Vascular Cognitive Impairment (TRACE-VCI) study is its enrollment of more than 800 subjects who have undergone MRI scans, a series of cognitive testing, and reviews of their vascular medical histories.
"The TRACE-VCI study will provide insight into the clinical features of memory clinic patients that meet vascular cognitive impairment criteria and establish key prognostic factors for further cognitive decline and (recurrent) major vascular events," wrote researchers, led by Dr. Jooske Marije Funke Boomsma from the Brain Center Rudolf Magnus Institute in Utrecht. "A strength of the TRACE-VCI study is that it addresses the clinical features and prognosis of VCI in a memory clinic setting, as there are few available cohort studies of VCI in this particular setting."
Previous research
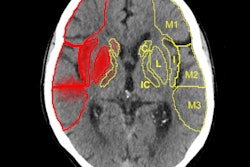
The majority of previous studies on the connection between vascular brain injury and cognition have centered on the general population and patients who experienced a stroke, transient ischemic attack, and myocardial infarction, or they have investigated only one type of vascular brain injury or condition, such as white matter hyperintensities.
"It is clearly important to document which clinical phenotypes related to vascular injury can be identified in a memory clinic setting and which factors determine prognosis for the individual patient," the authors noted (JMIR, 17 April 2017, Vol. 6:4, e60, pp.1-13).
This prospective observational follow-up study analyzed 861 consecutive patients suspected of cognitive impairment and who were referred to one of three outpatient memory clinics affiliated with the University Medical Center Utrecht and VU University Medical Center in Amsterdam. The subjects presented with cognitive complaints and vascular brain injury as seen on MRI scans during their first visits to the clinics between September 2009 and December 2013.
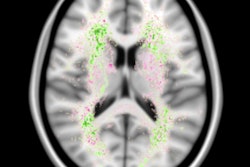
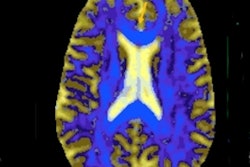
The vast majority (94%) of MRI scans were performed on 3-tesla systems (Signa HDxt and GE Discovery MR 750, GE Healthcare; Ingenuity, Achieva, and Ingenia, Philips Healthcare). MRI protocols included 3D T1-weighted, T2-weighted, T2- weighted/susceptibility-weighted imaging (SWI), and fluid-attenuated inversion recovery (FLAIR) sequences. A total of 850 (98%) patients were scanned using all of these sequences.
From the MRI results, the researchers visually assessed and rated medial temporal lobe atrophy (MTA) and white matter hyperintensities, both of which contribute to cognitive impairment.
| Vascular events and risk factors | |
| Patient demographics | No. of patients (%) |
| Male | 462 (54%) |
| Female | 399 (46%) |
| Mean age | 67.7 years (± 8.5) |
| Vascular risk factors | |
| Hypertension | 729 (85%) |
| Diabetes mellitus | 169 (20%) |
| History of reported vascular events | |
| Reported stroke | 78 (9%) |
| Reported vascular events other than stroke | 86 (10%) |
| Ischemic heart disease | 60 (7%) |
| Peripheral arterial disease | 31 (4%) |
Patients were divided into three categories of severity of cognitive impairment: dementia, mild cognitive impairment, and no objective cognitive impairment. They were deemed to have dementia if there was a cognitive deficit in at least two areas of neuropsychological testing and it interfered with daily functions. Mild cognitive impairment was seen as reduced cognitive function compared with baseline results. No objective cognitive impairment was having cognitive complaints, but there was no substantiated deficit on neuropsychological tests.
Patients also underwent a series of standardized cognitive assessments, which included an interview about their cognitive complaints, medical and family history, medication use, and education, as well as lifestyle habits, such as smoking, alcohol, and drug abuse.
In addition, they were asked to perform tasks to evaluate working memory, attention and executive functioning, processing speed, and perception.
Patient follow-up
Boomsma and colleagues reconnected with the subjects two years after initial baseline scans and tests. They conducted in-person clinic visits as well as phone interviews, if patients were unable to travel.
As the researchers performed their follow-up analyses, they were defining poor clinical outcome on several factors: noticeable cognitive decline; a major vascular event, such as a stroke, myocardial infarction, surgery, or endovascular treatment for coronary artery disease; and death.
"With regard to clinical phenotypes, it is important to know to which extent the type or location of vascular injury determines the cognitive profile," the authors noted. "This may support a more accurate diagnosis, particularly in the context of co-occurring neurodegenerative aetiologies, which will be much more common in memory clinic patients than in other populations."
Boomsma and colleagues noted several limitations of the pending results, including the inclusion of patients at tertiary referral facilities, "which may affect generalizability of the findings. Moreover, although patients were evaluated in a standardized fashion, the study does rely on data collection in the context of clinical care."
The latter limitation, they added, creates "some heterogeneity in data acquisition (e.g., MRI protocols) and not all parameters are available for all participants."
The researchers have almost completed the collection and processing of the final data, but they did not mention how soon the final study details would be released.