When integrated with prior clinical evaluation and exclusion of organic disease, pelvic MRI can play an invaluable role in the diagnosis, therapeutic guidance, and follow-up of pelvic floor dysfunction disorders, according to Portuguese researchers who received a coveted magna cum laude award at ECR 2017.
"MRI is a noninvasive, nonionizing radiation technique, which can be an important auxiliary tool for pelvic floor anatomy and functional evaluation, thanks to its extraordinary capabilities regarding tissue contrast," noted Dr. António Caetano and colleagues from Hospital Curry Cabral, Centro Hospitalar de Lisboa Central in Lisbon.
A common health problem
Pelvic floor disorders represent a common health problem, and can be exacerbated by issues such as advanced age, multiparity, obesity, smoking, previous pelvic surgery, constipation, genetic factors, and heavy physical exertion. The symptoms are variable and nonspecific, and clinical evaluation of these disorders is insufficient, the authors explained.
Radiologic evaluation should be preceded by a clinical history to include details on symptom duration and severity, physical examination, clinical background (obstetric trauma, surgery, inflammation, infections, inflammatory bowel disease, fistulas, etc.), colonoscopy/rectosygmoidoscopy, and functional and other tests.
"It is always imperative to exclude an organic cause, especially involving the colon and ano-rectal compartment," the researchers stated.
Among the advantages of MRI are its high contrast resolution (high spatial and temporal resolution) and multiplanar imaging capability, as well as the fact the technique is not limited by structure interposal, doesn't require retrograde opacification of the bladder, doesn't require fasting and intestinal preparation, is less operator-dependent than other exams, has high patient acceptance, allows for direct and integrated study of the pelvic compartments, and allows for a broader morphologic and dynamic study of the pelvic floor and the respective support system.
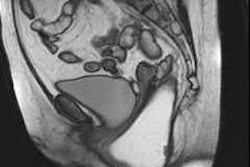
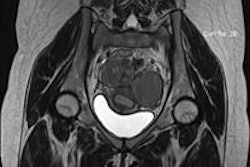
The pelvic compartments can be separated into three segments: anterior (bladder, bladder neck, uretra), middle (uterus, cervix, vagina), and posterior (sigmoid, rectum, anal canal). MRI permits evaluation of the three pelvic compartments, and often more than one compartment is affected.
Assessment of pelvic compartments with MRI defecography is a good option as it has a good interobserver correlation, the authors continued. It is indicated in cases where the patient complains or another exam suggests constipation, incontinence, defecatory dysfunction, rectal or anal pain, digitation, rectocele, enterocele, cystocele, and invagination or prolapse.
Optimum technique
The examination requires the use of a body phased-array coil. At Hospital Curry Cabral, it is performed in a closed 1.5-tesla MRI system. It is essential to explain the procedure fully to the patient, and to have access to clinical information.
Caetano and colleagues used a 50-cc syringe and a rectal catheter to inject ultrasound gel contrast. The amount of contrast introduced into the rectum varies between 150 and 250 cc, depending on the patient's tolerance. The patient should have a moderately filled bladder and stay in a supine position. They recommend using a disposable diaper.
| Summary of sequences used in MRI defecography | |||
| Sequence | Slice orientation | Matrix | Slice thickness |
| T1 TSE HR | Transversal | 320 | 3 mm |
| T2 TSE HR | Coronal | 384 | 3 mm |
| T2 TSE HR | Transversal | 384 | 3 mm |
| T2 TSE HR | Sagittal | 384 | 2.8 mm |
| T2 TRUFI - resting | Sagittal | 320 | 4.5 mm |
| T2 TRUFI - squeezing | Sagittal | 320 | 4.5 mm |
| T2 TRUFI Cine - defecation | Sagittal | 256 | 10 mm |
| T2 TRUFI defecation | Sagittal | 320 | 4.5 mm |
| T2 TRUFI postdefecation resting | Sagittal | 320 | 4.5 mm |
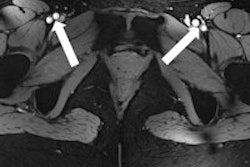
For anatomical evaluations, axial, coronal, and sagittal T2-weighted high-resolution images at rest are obtained for pelvic support elements (muscles, ligaments, fascias, bones), sphincteric components, organs (uretra, uterus, cervix, vagina, bladder, anal canal and rectum, in women).
For functional evaluations, T2 fast spin-echo and sagittal T2 cine MR acquisitions should involve resting, voluntary contraction of the perineum (valsalva and squeezing maneuvers), defecation (and maximum defecatory effort), and postdefecation resting.
Retention and evacuation of the pelvic organs requires structural and functional integrity of the pelvic floor elements, which include ano-rectal neuromuscular system, pelvic organs (bladder, uterus, and rectum), suspensory ligaments (anchorage points for muscles and viscera), muscles (support, contraction against ligaments, aperture/restraint), and osseous structures.
The pelvic floor unit is a multilayer system that provides active and passive support to the pelvic structures, and complex coordination and interaction are fundamental to pelvic floor function, the authors pointed out. The ligaments are formed from fascia thickenings, and both fascia and ligaments contribute to passive support of the pelvic structures. The active support of the pelvic floor depends on the pelvic muscular system. Undamaged structures are necessary for maintaining pelvic floor functional activity, and every pelvic compartment and structure is interdependent, interacting with and compensating for each other.
"Every study is made in the presence of the radiologist, who directs the exam and evaluates the images," the authors concluded. "In summary, MRI defecography allows for pelvic floor anatomy and functional evaluation, as well as their respective abnormalities, making a precise diagnosis, and provides valuable information on treatment planning."
To view their full selection of clinical cases and images presented at ECR 2017, click here.