The "gadolinium story" is the permanent talk of the town: In certain people, the injection of some gadolinium contrast agents can either lead to deposits of gadolinium in tissues or to severe, partly deadly side effects. I have been in the scientific gadolinium contrast agent business for more than 35 years and have summarized the history as I have witnessed it in a number of columns. The last and most factual report appeared in late 2015, describing the historical course of events as clearly as one can and asking the most important question: "Gadolinium: Will anybody learn from the debacle?"
The entire affair has been taken over by lawyers, judges, and health administrators and meanwhile its handling has completely gone off course. The companies and people involved seem not to want to collaborate but rather to fight each other. Some people are confused, some try to evade assuming any responsibility for what they have caused and whitewash themselves, some say it's an act of God, some try to make money -- while patients suffer and hardly anybody talks about them or tries to help.
 Dr. Peter Rinck, PhD, is a professor of diagnostic imaging and the president of the Council of the Round Table Foundation (TRTF) and European Magnetic Resonance Forum (EMRF).
Dr. Peter Rinck, PhD, is a professor of diagnostic imaging and the president of the Council of the Round Table Foundation (TRTF) and European Magnetic Resonance Forum (EMRF).The long-awaited decision of the London-based European Medicines Agency (EMA) on what should happen with linear gadolinium-based MR contrast agents is many months delayed, most likely due to objections by lobbyists. Meanwhile, the number of examinations with gadolinium contrast agents slowly declines and the indications are curtailed.
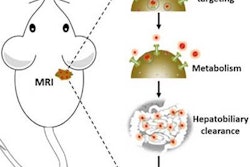
The odds are there will be drastic changes in contrast agent use already in the medium-term future. It seems as if manganese-based agents could replace gadolinium agents, at least for selected indications.
Manganese was the first element applied to enhance pathologies in MRI. Drs. Paul C. Lauterbur, Maria Helena Mendonça-Dias, and Andrew M. Rudin described its use in 1978.1 They imaged five dogs with myocardial infarctions after injecting a manganese salt solution and were able to highlight the lesions.
Gadolinium became the element of choice for MR contrast agents because of its high relaxivity and patent issues, but it is an element foreign to the human body, whereas manganese is an essential trace element.
The only manganese-based agent approved and sold for clinical imaging was Teslascan (Mn-DPDP), a compound used for liver imaging. Because it didn't sell for the indication, it was withdrawn from the market some time ago.
In addition to imaging of the liver, manganese-enhanced MRI (MEMRI) with Mn-DPDP has a wide range of potential applications. Research is focused upon both depiction of brain damage and functional mapping of neural pathways to map brain activation independently and with higher contrast than measurements of hemodynamics in functional MRI.
Contrary to gadolinium-based compounds, which are unspecific agents, manganese agents can actively track biological processes. Manganese also has an affinity for the myocardium and can act as a biomarker in heart disease. It competes with calcium for entry into cardiac cells. There, its ions bind to macromolecules and influence the relaxation of cell and tissue water. Heart diseases gradually inactivate calcium transport mechanisms, due to lower metabolic activity. Thus, manganese uptake is reduced accordingly; manganese-induced changes of tissue relaxation reflect quantitatively tissue calcium homeostasis and thus myocardial viability.2,3
During the development of Mn-DPDP as an MR contrast agent for liver studies, researchers discovered that this compound and its metabolite, manganese pyridoxyl ethyldiamine (Mn-PLED), also possess therapeutic properties. Mn-DPDP has been studied in cancer patients and in patients with myocardial infarctions. The contrast enhancement in MRI relies on the release of manganese from the chelate, the therapeutic activity depends on manganese that remains bound to DPDP or PLED.
Mn-PLED's stabilized derivate calmangafodipir [Ca4Mn(DPDP)5] has even superior therapeutic properties.4 MEMRI of the heart is a good example of one of the few promising molecular imaging methods, because the same manganese-based compound can be used for diagnostics and treatment of, e.g., myocardial infarctions, cancer, and drug intoxication (theragnostic properties), is inexpensive, and addresses a mass market.
Overall, the situation not only represents a reshuffle of the deck of cards -- some of the players will leave the card table and will be replaced by others. Small startups seem to liaise with distributors without an R&D department of their own, whereas the former big players seem to adopt a wait-and-see attitude.
Dr. Peter Rinck, PhD, is a professor of diagnostic imaging and the president of the Council of the Round Table Foundation (TRTF) and European Magnetic Resonance Forum (EMRF).
References
- Lauterbur PC, Mendonça Dias H, Rudin AM. Augmentation of tissue proton spin-lattice relaxation rates by in vivo addition of paramagnetic ions. In: Dutton PO, Leigh J, Scarpa A (eds). Frontiers of Biological Energetics. New York: Academic Press, 1978:752-759.
- Skjold A, Amundsen BH, Wiseth R, Støylen A, Haraldseth O, Larsson HB, Jynge P. Mangenese dipyridoxyl-diphosphate (MnDPDP) as an in vivo viability marker in patients with myocardial infarction. J Magn Reson Imaging, 2007;26:720-727.
- Pan D, Caruthers SD, Senpan A, Schmieder AH, Wickline SA, Lanza GM. Revisiting an old friend: Manganese-based magnetic resonance imaging contrast agents. Wiley Interdisciplinary Reviews: Nanomedicine and Nanobiotechnology, 2010;3:162-173.
- Karlsson JOG, Ignarro LJ, Lundström I, Jynge P, Almén T. Calmangafodipir [Ca4Mn(DPDP)5], mangafodipir (MnDPDP) and MnPLED with special reference to their SOD mimetic and therapeutic properties. Drug Discovery Today, 2015;20(4):411-421.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnieEurope.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.