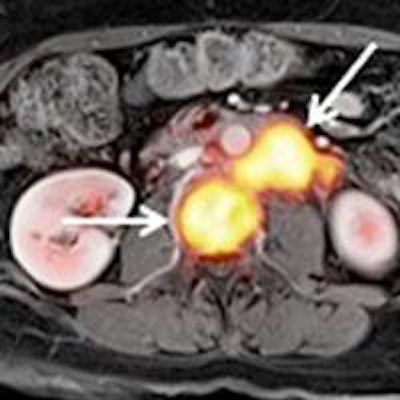
PET/MRI is a valuable tool to accurately stage tumors of the uterine cervix and may serve as an alternative modality for a clinical workup prior to treatment, according to a German study presented at the recent RSNA 2016 meeting in Chicago.
Researchers, led by Dr. Johannes Grueneisen from Essen University Hospital, found that PET/MRI detected all but one primary tumor among patients with uterine cervix cancer and achieved greater sensitivity, specificity, and diagnostic accuracy than MRI alone for identifying positive lymph nodes.
The findings demonstrate the usefulness of FDG-PET as a "valuable additive to MR imaging for more accurate nodal staging of patients with cervical cancer," he noted.
PET/MRI's utility
Over the last four or five years, molecular images from PET and high-resolution anatomical MR images of soft-tissue contrast have made the hybrid modality appealing to clinicians for a variety of applications. Grueneisen and colleagues have been active in exploring the efficacy of PET/MRI in women's oncological imaging.
 Dr. Johannes Grueneisen from University Hospital Essen.
Dr. Johannes Grueneisen from University Hospital Essen.Last year, the researchers concluded the hybrid modality provided high diagnostic performance for restaging gynecological cancer patients compared with FDG-PET/CT, with only slightly longer scan time and "markedly reduced" radiation exposure.
Two years ago, the Essen group concluded that adding diffusion-weighted imaging (DWI) to FDG-PET/MRI to stage women with primary or recurrent pelvic malignancies contributed minimal value and is not worth the additional scan time. As a follow-up to those papers, Grueneisen and colleagues expanded their evaluation of PET/MRI to uterine cervix cancer patients.
The researchers prospectively enrolled 44 consecutive patients with histopathologically verified primary cervical cancer. All patients underwent a whole-body PET/MRI scan prior to the initiation of treatment or surgery on an integrated system (Biograph mMR, Siemens Healthineers). MRI sequences included T2-weighted half-Fourier acquisition single-shot turbo spin-echo (HASTE), DWI, and postcontrast T1-weighted volumetric interpolated breath-hold examination (VIBE), along with a dedicated MRI protocol for the female pelvis for delineation of the extent of local tumor.
A radiologist and nuclear medicine physician interpreted the results by first reading MR images only, then viewing the PET/MRI image sets. They were asked to determine the extent of local tumors to identify potential tumor invasion inside the adjacent pelvic organs and to determine the T-stage and the occurrence of lymph nodes or distant metastases.
For the reference standard, researchers took into account characterizations of all histopathological samples of the primary tumors and lymph nodes. If and when only histopathological information was included in a patient's study, a follow-up CT or PET/CT was used for reference.
Tumor assessments
The combination of PET/MRI accurately detected 43 (97%) of the 44 primary cervical tumors. The one omission undiscovered by the hybrid modality was a tumor classified as stage IA under International Federation of Gynecology and Obstetrics (FIGO) guidelines. In addition, both, MRI and PET/MRI correctly determined the tumor stage in 38 (86%) of the 44 patients.
In addition, lymph node metastases also were found in 19 (43%) of the 44 patients. In this evaluation, PET/MRI achieved greater sensitivity, specificity, and diagnostic accuracy compared with MRI alone for identifying nodal-positive patients.
| Detection of lymph node metastases | |||
| Sensitivity | Specificity | Accuracy | |
| PET/MRI | 84% | 92% | 89% |
| MRI | 68% | 87% | 80% |
Both PET/MRI and MRI alone successfully found distant metastases in three patients.
While FDG-PET did not necessarily add any additional information to MRI for identifying the spread of local tumors, the combination of MRI and simultaneous PET advances the evaluation of uterine cervical cancer and could become a "valuable alternative/adjunct for the clinical workup in a pretreatment setting," he added.