
Breast cancer screening has been a topical issue at the Journées Francophones de Radiologie (JFR) meeting, which concludes today in Paris. It enjoyed extensive coverage in Friday's opening press conference, and it's significant that JFR 2016 take place bang in the middle of France's national month of breast cancer screening awareness, Pink October.
During the congress, Pink October has attracted publicity as part of a campaign that serves to not only raise public awareness, but also refocus scientific debate.
 A one-day diagnostic turnaround in a screening institute requires a specialized breast multidisciplinary team to be on hand for all steps of the process, said Dr. Suzette Delaloge. Image courtesy of Gustave Roussy Institute.
A one-day diagnostic turnaround in a screening institute requires a specialized breast multidisciplinary team to be on hand for all steps of the process, said Dr. Suzette Delaloge. Image courtesy of Gustave Roussy Institute.On Friday, Dr. Suzette Delaloge, head of the breast pathology committee at Gustave Roussy Institute (Institut Gustave Roussy, IGR), in Paris outlined the institute's "one-day diagnosis plan" in breast cancer screening that it has championed since 2004. Dedicated to women with a suspicious breast lesion, this speedy diagnostic process requires the collaboration of a multidisciplinary team specialized in the breast. If the lesion is benign, reassured patients can return home the same day. In the opposite case, the multidisciplinary team will meet so a therapeutic plan can be put to the patient. The concept of the "one-stop clinic" compares favourably with the traditional diagnostic route, which can take days if not weeks, according to Delaloge.
Initially a concept for symptomatic lesions in the 1990s, the idea was extended in 2004 to all suspicious lesions detected during screening of targeted women ages 50 to 74. Since the launch of this extended strategy, more than 14,000 women, 80% living in Paris, have visited the one-day clinic and an average of 28 patients are seen each day. The question is: How can such a one-stop shop for breast cancer screening be replicated?
France's National Cancer Plan stipulates that a multidisciplinary team grouped in the same structure is essential for assessing the different parameters of diagnosis and agreeing on the best therapy. At IGR, the team comprises a breast surgeon, oncologist, radiologists, and a specialized cytopathologist, with coordinating support from other medical and nonmedical staff.
Assessment of breast masses involves clinical examination, a complete review of existing images, and new imaging procedures, plus image-guided biopsy. The team routinely uses ultrasound-guided fine needle aspiration, angiomammography, and CT if necessary. Workup is completed through ultrasound-guided biopsy if needed, according to Delaloge.
A recent study published in the European Journal of Cancer confirmed the cost-benefits of the one-day clinic at IGR, and calculated the median cost of a diagnostic procedure to be 420 euros. To assess the one-day diagnostic strategy, the study analyzed 10,692 patients seen at the center between 2004 to 2012, and compared results of the one-day diagnosis with result confirmation after surgery, biopsy, or long-term monitoring.
The study confirmed in initial diagnosis, benign lesions represented 56% of diagnoses, 36% of lesions were considered malignant, 5% suspicious or atypical, and only 3% could not be interpreted. Furthermore, 69% of women had a mass, 31% microcalcifications or other types of lesions. In 75% of cases, an accurate diagnosis could be established in a day, which rose to 87% if the mass was detected clinically or by mammography. Sensitivity of diagnosis was estimated at 98.4% and specificity was deemed 99.8% with a positive predictive value of 99.7%.
FNMR presence
Pink October's breast screening awareness campaign has morphed into various forms. In a striking visual flier, designed to grab women's attention, the National Union of Independent Radiologists (Fédération Nationale des Médecins Radiologues, FNMR) asks, "When was your last mammography test?" while reminding them there are 4,800 private radiologists across France waiting for their visit -- which in France's national screening strategy should be every two years after the age of 50. The visual also provides a link for further information, and calls on the authorities to support efforts by independent practitioners to maintain an accessible and quality service.
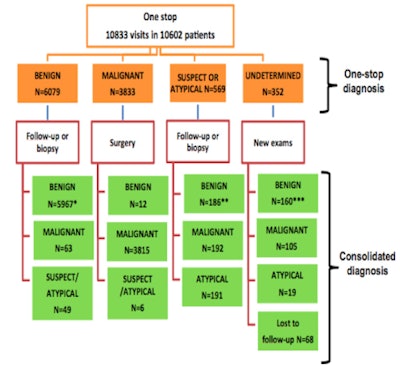 Diagnostic pathways and consolidation of the diagnosis.
Diagnostic pathways and consolidation of the diagnosis.The publicity has emerged in tandem with a 140-page report from a breast cancer screening steering committee comprising stakeholders in the medical and governmental sectors who call for improvements in the detection of breast cancer. Committee members include medical and managerial representatives from various cancer, epidemiological, biostatistical, and public health institutes, as well as general practitioners (GPs) and professors from medical science departments.
Excluded from consultation
The report, which was supported by France's National Cancer Institute (INCa), has received a mixed response from the majority of radiologists who claim they were not consulted during its preparation.
The document's opening statements allude to the controversy that continues to dog screening programs today, namely doubts of how much the risk of death from breast cancer is reduced, and the fear of overdiagnosis and overtreatment. It also points to a range of very disparate results from international studies about risk and overdiagnosis, and raises the issue of anomalies and dysfunction in the current organization of screening.
Such problems have resulted in unequal access, a lack of comprehension of screening issues, confusion between primary prevention, screening, and early detection, and an absence of GPs in the process of organized screening, according to the report. The document also states such problems are compounded by misleading and excessive marketing of Pink October, and specifically for the patients, by partial and poorly explained reimbursement of ultrasound, and doubts surrounding certain therapeutic strategies.
Through consultation, the committee has come up with several recommendations that it believes will significantly improve the current situation, which the committee said is not fit for purpose as a screening proposal for healthy women. One senior radiologist commented that importantly the recommendations underlined the importance of getting GPs actively involved in discussion of screening with healthy patients.
The report also outlines two possible scenarios for the future. The first scenario is the screening program is stopped because mammography is deemed a tool to use only in the management of individual patients. The second scenario also envisages a stop to the existing program, but also the implementation of a new drastically revised screening program.
The two scenarios reflect the diversity of opinion within the committee, according to the report, which states the committee will not take sides either way but hopes improvement will quell current controversy and restore confidence in the mechanism chosen for optimal breast cancer detection and management.
Report recommendations
The committee recommends the following:
- Consideration should be taken of the controversies with regard to screening, both in the information provided to women and in the information and training (initial and continuous) of professionals, so women eligible for breast cancer screening receive full and balanced information and also so the screening staff can develop relevant knowledge in order to adequately support women as they make informed decisions.
- The improvement of scientific knowledge about breast cancer and carrying out an ambitious evaluation about the strategies already in place or to come, through implementation of research projects that study the natural history of breast cancers and their nature, in order to better differentiate types of cancer and their potential evolution; and implementation of state-of-the-art system of information and monitoring to allow a permanent evaluation of programs.
- Evolution of breast cancer screening to allow the integration of the GP in the screening strategy while also factoring in other health professionals such as midwives and gynecologists; double reading of all screening mammograms. It is not acceptable that two screening systems coexist with different criteria; evaluation of ultrasound to complement mammography; the cessation of all early screening for women under 50 and for women at low risk, this through implementing a strategy of nonreimbursement for the act.
- The integration of breast cancer screening strategies in a wider prevention and screening strategy through implementation of a tailored consultation. The consideration of the individual will allow a more adapted follow-up for everyone. Breast cancer screening that is divorced from other screening and prevention processes does not make much sense in terms of public health.
- The development of a breast cancer screening and follow-up strategy that is based on risk factors. It is possible with development of knowledge of blood markers researchers will be able to identify higher-risk as well as low-risk women, obviating the need for participation in screening programs as they are known today. This requires deployment of an identification system for risk levels and implementing follow-up in line with validated recommendations. There should also be an evaluation of recommendations and high reactivity level to recommended action, in line with the development in knowledge, and evaluation results.



















