To help eliminate mistakes by radiology trainees reporting out-of-hours cervical spine trauma CT scans, it's crucial to bear in mind seven key learning points, U.K. researchers reported at the 2016 congress of the European Society of Musculoskeletal Radiology (ESSR 2016).
There is an ever-increasing demand on trainees to promptly and accurately report emergency CT scans of the cervical spine following trauma, explained Dr. Sheetal Bhushan Gagrani, a radiologist in the imaging department at Leicester Royal Infirmary in Leicester, U.K. To expedite patient care and cut errors, the following tips and tricks are recommended:
- Use all the reconstructions available to you -- axial, coronal, and sagittal. Ask radiographers for thinner slices if you don't see an acute fracture but there is a high clinical index of suspicion.
- Scrutinize the images in front of you. Use a systematic approach, as when reporting any image.
- Understand the anatomy of the spine. It is important to localize the fracture into the appropriate spinal columns. This assists in deciding on the significance and stability of the patient's injury.
- Understand the anatomy associated with the spinal column. Determining the location of fractures helps convey to the clinician the stability of the patient's injury.
- Fractures can present primarily as subtle linear defects, with no evidence of displacement. Ensure you understand the normal vascular markings and how these differ from fracture lines in order to allow differentiation between the two.
- Understand the common fractures that present in the cervical spine (Jefferson's, hangman's, clay shoveler's) and injuries secondary to these you should inspect for.
- Your review areas should include the facet joints (look out for subluxation/dislocation), the occipital condyles, foramen transversarium, and the imaged part of the lower skull.
"It is imperative to provide adequate training, identify common mistakes, and the cause for the mistakes prior to starting on call," noted Gagrani and colleagues in an e-poster at ESSR 2016. "Residents' reports are reliable and with low errors and discrepancy rates."
CT scans of the cervical spine following trauma is one of the most common investigations performed in any emergency radiology department, and in most institutions, radiology residents provide out-of-hours interpretation of posttraumatic cervical spine CT scans, with reports being subsequently checked and verified by specialist radiologists, they stated. Timely and accurate interpretation of the CT scans plays an important role in patient treatment and outcome following cervical spine injury.
"Discordant reports between radiology residents and consultant radiologists can occur due to a variety of factors. These include cognitive, perceptual, and communication errors as well as satisfaction of search," the authors wrote, adding that previous studies have demonstrated overall CT discrepancy rates of between 8% and 25%, with major amendments recorded as being between 0.8% to 10%.
Unearthing major discrepancies
They analyzed a retrospective database of cervical spine CT scans reported by residents out of hours using the RIS between November 2014 and November 2015. Out of hours was defined as between 5 p.m. and 9 a.m. and weekends. The discrepancies were graded as minor, significant, and major.
A major discrepancy was regarded as having an adverse effect on patient outcome, requiring a change in management, and causing significant morbidity or mortality. Significant discrepancy was regarded as having an impact on patient management but did not contribute to long-term morbidity. Minor discrepancy was regarded as having no impact on the clinical management of the patient.
The level of training of residents and the radiologist-specific causes such as cognitive (misinterpretation), observational (complete miss), or satisfaction of search were documented according to the U.K. Royal College of Radiologists' (RCR) standards for learning from discrepancies meetings. The findings were independently verified by two experienced musculoskeletal radiologists.
A total of 630 CT scans were reported by radiology residents out of hours. There were 34 discrepancies, giving a discrepancy rate of 5.4%. There were three major (0.5%), 14 significant (2.2%), and 17 minor (2.7%) discrepancies. Radiologist-specific causes included 11 cognitive, 18 observational, and six satisfaction-of-search errors. There were three false-positive errors. No significant difference in discrepancy rate was identified for various levels of training.
The three major discrepancies occurred in the following cases:
- A 79-year-old woman with a known history of osteoporosis fell down five steps. She complained of immediate neck pain. Clinical examination revealed C2 tenderness. The CT cervical spine was reported as normal by the radiology resident on call. Checking and verification of the scan by the consultant revealed a fracture through the right C4/5 facet joint with widening, a fracture through the left C5 foramen transversarium, and clay shoveler's fractures at C4 and C5.
- An 81-year-old man who presented to the accident and emergency department with neck pain and multiple areas of bruising to the head after a fall whilst he was intoxicated. He was tender at C5-C7. The cervical spine CT was reported as normal by the radiology resident. Checking of the scan by the consultant radiologist demonstrated a fracture through the right C5 foramen transversarium.
- A 35-year-old woman was involved in a road traffic accident. She had a whole-body trauma CT scan. The radiology resident reported the CT cervical spine as normal. Checking by the consultant radiologist revealed an undisplaced fracture through the left occipital condyle.
For more details and to view the authors' clinical cases presented at ESSR 2016, click here.
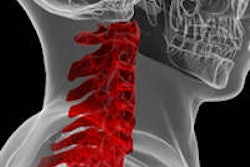
Editor's note: The image on the home image shows dislocation injury to the cervical spine after road traffic accident with permanent high paraplegia. Image courtesy of Dr. Stefan Wirth.