Dutch researchers are using a novel approach to radical prostatectomy by combining a hybrid imaging agent with SPECT/CT to detect lymph nodes and guide robot-assisted surgery, according to a study in the July issue of the European Journal of Nuclear Medicine and Molecular Imaging.
While there is hope the technique eventually could be beneficial, early results show deficiencies, and more technological improvements must be made to advance the use of robot-integrated guidance modalities in surgical procedures (EJNMMI, July 2016, Vol. 43:7, pp. 1,278-1,287).
"Hybrid tracers help to integrate nuclear medicine and fluorescence-guided robotic surgery, but the use of a robot-integrated fluorescence laparoscope did not improve fluorescence-based sentinel lymph node identification," the authors noted. "Further technical refinement of robot-integrated guidance modalities in surgical procedures should improve the relationship between preoperative and intraoperative imaging findings."
Robotic surgery
Dr. Gijs H. KleinJan, a PhD student at the Interventional Molecular Imaging Laboratory at Leiden University Medical Hospital, and colleagues, explained that robot-assisted approaches to radical prostatectomy and complementary extended pelvic lymph node dissection of sentinel lymph nodes and nonsentinel lymph nodes are becoming more in vogue as the technology becomes more sophisticated.
It is believed one key component to making this approach successful is the integration of fluorescence guidance technologies and novel radiotracers to enhance robot-assisted surgeries.
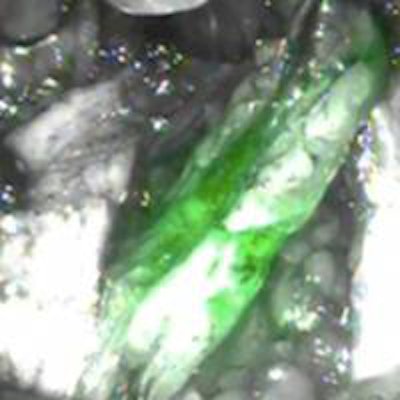
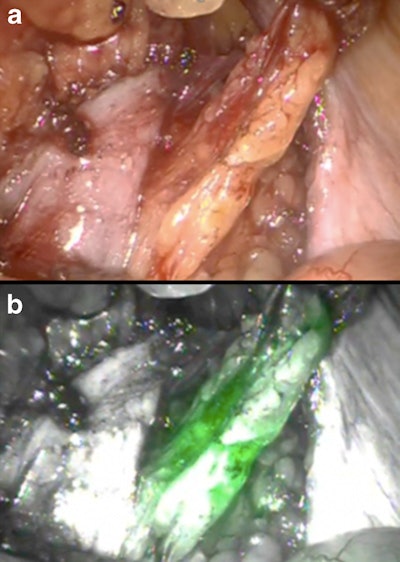 Fluorescence-based images show locations of sentinel nodes and lymph nodes (a and b) detected intraoperatively inside and outside the extended pelvic lymph node dissection area (green in vivo fluorescent sentinel nodes, yellow ex vivo identified sentinel node). Images courtesy of EJNMMI.
Fluorescence-based images show locations of sentinel nodes and lymph nodes (a and b) detected intraoperatively inside and outside the extended pelvic lymph node dissection area (green in vivo fluorescent sentinel nodes, yellow ex vivo identified sentinel node). Images courtesy of EJNMMI.In this case, Dutch researchers utilized a hybrid fluorescent radioactive tracer known as indocyanine green-Tc-99m-nanocolloid, which was introduced in 2009 for sentinel node biopsy.
The hybrid tracer is used with a fluorescence laparoscope to preoperatively detect and map sentinel lymph nodes in real time. However, the drawback is that a bedside assistant often has to control the fluorescence laparoscope, rather than the operating urologist.
"We thus hypothesized that use of a robot-integrated fluorescence laparoscope could increase the level of control the operating urologist has, and could thus help increase the success rate in resecting preoperatively identified sentinel lymph nodes via fluorescence guidance," the authors wrote.
Patient evaluations
Between January 2014 and July 2015, researchers enrolled 50 patients with lymph node metastases and added five patients from July to September 2015 as a subgroup.
All 55 patients were scheduled for robot-assisted radical prostatectomy, extended pelvic lymph node dissection, and sentinel lymph node removal with the hybrid radiotracer and SPECT/CT as one way to detect the abnormalities.
The first 50 subjects underwent preoperative robot-integrated fluorescence laparoscope using standard settings, while the additional five patients received the same procedure with customized fluorescence imaging settings.
In the five-person subgroup, the intensity of the white light background in the fluorescence image varied from the standard setting of 30% down to 15% and 0%, so the visibility of the fluorescence signal within the sentinel lymph nodes could be evaluated at the three different settings.
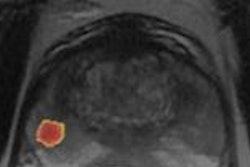
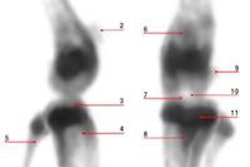
Preoperative lymphoscintigraphy was performed 15 minutes and two hours after tracer injection, while SPECT/CT imaging occurred directly after acquisition of the second lymphoscintigrams to further detect and record the number and location of sentinel lymph nodes.
The information from the SPECT/CT images then helped guide the robotic surgical device (da Vinci, Intuitive Surgical), along with the fluorescence laparoscope for optimal sentinel lymph node localization and resection.
Preoperative discoveries
Researchers preoperatively detected 147 sentinel lymph nodes on the lymphoscintigrams from the entire cohort of 55 patients, with 65 more sentinel lymph nodes found through SPECT/CT, bringing the total number to 212 sentinel lymph nodes (median of four nodes per patient).
Of these 212 sentinel lymph nodes, 55 nodes (26%) were located outside the extended pelvic lymph node dissection area.
Intraoperative fluorescence imaging using standard settings uncovered 148 (80%) of 184 sentinel lymph nodes among the initial 50 patients. The percentage of detected sentinel lymph nodes increased to 86% (12 of 14 sentinel lymph nodes) through the customized fluorescence settings among the smaller subgroup.
Of the 201 sentinel nodes identified in the initial 50 patients on preoperative SPECT and hybrid tracer imaging, 36 nodes (18%) were not removed due to their anatomical location or close proximity to other structures, such as the rectum, or behind vascular structures.
"In the remaining patients, the anatomical locations derived from the SPECT/CT images were used to position the fluorescence laparoscope or, when intraoperative fluorescence imaging did not provide accurate sentinel node identification, to guide resection of the sentinel nodes," the authors wrote.
A total of 148 (80%) of the 184 sentinel lymph nodes were removed using intraoperative fluorescence guidance. An ex vivo analysis of the extended pelvic lymph node dissection found that fluorescence identified 180 (97%) of the 184 sentinel lymph nodes resected, and the radioactive signal from the hybrid tracer was evident in 100% of the sentinel lymph nodes.
Based on the results, Dutch researchers concluded the combination of 3D preoperative SPECT/CT with the hybrid tracer with the robotic fluorescence laparoscope improved the surgeon's use of the technology and did not influence the sensitivity or morbidity of the procedure.
"To our surprise, however, the detection rates with the current fluorescence camera did not improve," they stated. "Hybrid tracers help to integrate nuclear medicine and fluorescence-guided robotic surgery, but the use of a robot-integrated fluorescence laparoscope did not improve fluorescence-based sentinel lymph node identification."
They hope additional technical improvements of robot-integrated guidance modalities in surgical procedures will "improve the relationship between preoperative and intraoperative imaging findings."