A leading facility in France is shaking up how it approaches breast cancer with surprising results. The "one-stop clinic" model is a multidisciplinary team approach that reportedly generates high sensitivity and specificity -- nearly 100% -- as demonstrated by 8.5 years of data.
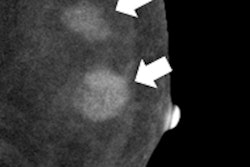
Approximately 11,000 women have visited Institut Gustave Roussy (IGR) in Villejuif, south of Paris, in the last 8.5 years. Patients with an abnormal mammogram or suspected lesions (BI-RADS 3, 4, 5) are referred to the clinic and meet with an oncologist, surgeon, and radiologist as necessary. Approximately 75% of patients receive same-day results of a mammogram, ultrasound, digital breast tomosynthesis (DBT) exam, contrast-enhanced spectral mammogram (CESM), or fine-needle aspiration (FNA) biopsy. Afterward, the patients receive diagnosis and treatment planning.
Reportedly, the clinic has a sensitivity of 97% and a specificity of 99.7%.
Why this approach?
In 2004, France launched a national screening program, without a clearly organized postscreening model.
"At that time, nationwide, postscreening diagnostic time intervals were high, even at our institution," said Dr. Suzette Delaloge, associate professor of medical oncology and head of the breast cancer department at IGR and chair of the French National Breast Cancer InterGroup-Unicancer. "With that in mind, coupled with in France alone, each year, 49,000 new breast cancer cases being diagnosed, we took a close look at how we could develop a program that would deliver on the unmet need for faster diagnosis and treatment planning."
The goal was to create an environment for patients where they would experience shorter time intervals between "positive" screening and diagnosis, coupled with accuracy and high-quality care. From there, they developed a model for the one-stop clinic.
Since its launch, the clinic has added CESM and DBT, which can decrease the number of false positives compared with regular mammography, according to Delaloge's colleague Dr. Clarisse Dromain.
Can others adopt this model?
It would be a mistake to think the clinic's model of a "one-stop shop" can be copied and pasted other places, according to Catherine Tabaka, chief marketing officer of women's healthcare at GE Healthcare, a long-standing partner and equipment provider to IGR.
"The 'secret sauce' of the multidisciplinary team is what allows 75% of women to leave with a treatment plan," she said in an interview with AuntMinnieEurope.com. "The secret sauce leads to diagnosis accuracy," not a single piece of equipment. GE is not touting the one-stop clinic as a worldwide solution.
"It takes a lot of effort," she said. "It's a constant revisiting and asking how to improve, which is why CESM and DBT were added to the portfolio. The multidisciplinary team is the success. A lot of personnel are brought together in a bubble and the one-stop shop works well to help patients progress through the process with the right pace with the right decision-making."
A lot of other hospitals and private clinics have replicated this organization, but the main difficulty for the implementation is to find a pathologist with enough experience in breast lesion cytology that is really different from breast lesion histology, according to Dromain.
"Indeed, the diagnostic performance should be very high to avoid false-negative interpretations as well as false positives," she told AuntMinnieEurope.com. "In IGR, to consolidate this risk we have decided to perform a biopsy in addition to the FNA in each case of discordance between the radiological interpretation and the cytology results. We also have six-month follow-up for all patients for whom a benign lesion has been diagnosed."
To overcome this problem, some other hospitals have developed similar approaches based on fast biopsy instead of FNA, she said.
"However, in this case, it's difficult to have the final diagnosis in less than 48 hours," she added. "The other difficulty is to be able to regroup a multidisciplinary team of experts of different specialties (oncologists, surgeons, radiologists, pathologists) on the same day."
The one-stop clinic model is indicative of a broader transformation in women's healthcare, according to Tabaka.
"People want to make better sense of and to better organize their process in the most effective and efficient way," she said. "It is about clinical outcome, the right answer in delivering diagnosis -- only calling back those who need to be seen again. The real breakthrough is to organize a set of tools to give a level of confidence in timely manner -- not agonize for three weeks or a month for an answer."