Usually benign imaging findings may hide a malignant lesion such as medullary carcinoma, so it's vital to be aware of these "false friends," according to researchers from Madrid who have provided some tips and tricks in award-winning work.
The relationship between mammograms, ultrasound, MRI features, and pathologic findings in benign-looking malignant lesions were analyzed by Dr. Rosa Lorente Ramos, PhD, from the Unidad Central de Radiodiagnóstico (UCR) de la Comunidad de Madrid, and colleagues.
"Although the majority of breast carcinomas show malignant features at imaging, benign-looking malignant lesions may appear, causing a delay in correct diagnosis and treatment," they noted in an e-poster from RSNA 2015 that earned a certificate of merit and received 60 likes.
These are their top tips for dealing with benign-looking findings:
- All breast masses should be carefully assessed, looking for subtle findings on mammograms and ultrasound and compared with previous studies. Some of them may be tricky and malignant, despite a benign-looking appearance.
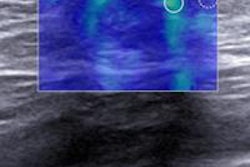
- Acoustic enhancement on ultrasound in a solid lesion may be caused by areas of mucin.
- Medullary carcinoma presents as circumscribed margins and is usually homogeneous due to high cellularity caused by lymphoplasmacytic infiltration.
- Papillary carcinoma: gross specimens are round, well-defined nodules composed of low-grade ductal cells separated by fibrovascular cores or vascular channels. Hemorrhage is frequently present.
- Abscesses are lesions with posterior acoustic enhancement, low-level content, but sometimes thick-walled or mixed masses with circumscribed margins.
- Inflammatory signs may not be evident.
- Follow-up after treatment reveals resolution. Neoplasms may also be infected.
- Cystic areas are more frequent in malignant phyllodes tumors than in benign phyllodes tumors and fibroadenomas.
- Lesions growing in size should be biopsied and sometimes excised. Benign and borderline phyllodes tumors are difficult to diagnose, sometimes resembling fibroadenoma even on biopsy.
- Malignant lesions and even big, rapidly growing masses may appear well-circumscribed, depending on the growth pattern.
Breast cancers usually appear on mammography, ultrasound, and MRI as irregular noncircumscribed masses, with or without microcalcifications, the authors explained. However, in 10% to 20% of cases, breast cancers may show a benign-looking appearance, presenting with well-circumscribed breast masses. Malignancies that most frequently appear with a benign appearance include mucinous or colloid carcinoma, medullary carcinoma, papillary carcinoma and malignant phyllodes tumors. Also, invasive ductal carcinoma may present with a falsely benign imaging appearance.
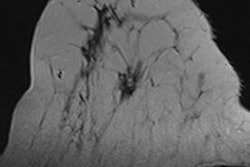
On mammography, breast malignancies may present with nonaggressive features. Lorente Ramos and colleagues recommended looking for subtle findings on mammograms and to compare them with previous studies, where important clues could be found such as a new lump or a mass that may hide a malignancy.
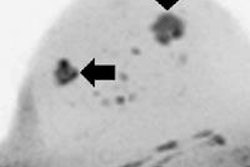
On ultrasound, medullary, mucinous, and papillary carcinoma, as well as malignant phyllodes tumors, usually present with large cystic areas due to necrosis or colloid content. On ultrasound, they are complex masses, mixed solid and cystic masses, or cysts with nodular-appearing solid area. Masses with more than 50% solid area are suspicious, but even smaller solid areas may be malignant. The solid area should be biopsied, according to the researchers.
MRI can help to evaluate breast masses, which is especially useful in difficult cases. Analysis of the lesion on signal intensity on T2-weighted MR images, assessment of the enhancement pattern, and kinetic curve help in differentiating between malignant and benign well-circumscribed breast lesions.
Practical tips on biopsies
The researchers also presented a second e-poster on radiologic-pathologic discordances in core biopsy. They found the main reasons for discordance were difficult biopsy technique, difficult histopathology, missing calcifications, and difficult correlation.
Some of their tips are listed below:
- Turn the patient on her side to achieve a better approach.
- Infiltrating the anesthesia beneath the lesion may make it more superficial. It will also prevent anesthesia from obscuring the lesion.
- The needle tip should always be visualized to avoid complications.
- Multiple biopsy passes should be obtained from different areas of the lesion.
- Remember to always keep the needle parallel to the transducer.
- Benign lesions do not require surgery; if sampling is wide on biopsy, a close follow-up may be performed. Atypia may appear on core biopsy requiring surgery.
They also remind physicians not to try to diagnose everything on a biopsy because the main aim of a core biopsy is to suggest the correct management of that lesion.