Ultrasound can be used to identify subclinical disease activity in rheumatoid arthritis (RA) patients in remission, enabling them to benefit from more-intensive treatment, according to research presented recently at the European League Against Rheumatism (EULAR) annual congress in Rome.
The results included preliminary data from the Sonographic Tenosynovitis Assessment in Rheumatoid Arthritis Patients in Remission (STARTER) study. The Musculoskeletal Ultrasound Study Group, part of the Italian Society of Rheumatology, reported that ultrasound diagnosis of synovitis and, for the first time, tenosynovitis was associated with RA flare in nonsymptomatic patients. Notably, ultrasound diagnosis of tenosynovitis was more specifically associated with flare and the need to increase treatment, according to the researchers.
"[Musculoskeletal ultrasound] assessment of tendons should be a part of the evaluation and might help [to] better stratify RA patients in clinical remission," said presenter and co-principal investigator Dr. Emanuela Bellis of the Ospedale Mauriziano in Italy.
Similarly, in another study presented at EULAR 2015, researchers in Japan found that providing intensive treatment for patients with subclinical active synovitis identified on power Doppler ultrasound could prevent the progression of joint damage.
Tenosynovitis
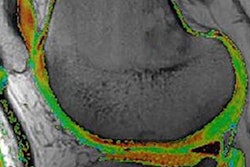
While the goal of treating rheumatoid arthritis is to achieve remission, subclinical disease activity may still persist in these patients. Synovitis detected on power Doppler ultrasound has been shown to be a valid measure of subclinical inflammation, but the frequency and clinical significance of subclinical tenosynovitis is not well-understood, according to the Italian researchers.
The group aimed to estimate the prevalence of musculoskeletal tenosynovitis diagnosed by ultrasound in patients in clinical remission, and to compare the association of tenosynovitis and synovitis with flare, functional disability, and damage. All members of the Italian Society of Rheumatology were invited to participate in the study, and 35 investigators from 25 centers signed on.
Consecutive RA patients in clinical remission were recruited from January to June 2014; they received a full clinical evaluation and ultrasound to assess synovitis and tenosynovitis at the wrists, hand and finger joints, and extensor/flexor tendon sheets. Of the 427 patients in the study, approximately 50% showed tenosynovitis on baseline grayscale ultrasound, and approximately 20% demonstrated tenosynovitis on baseline power Doppler ultrasound. Tenosynovitis on power Doppler ultrasound was most associated with patient-reported unstable disease at baseline, the researchers noted. Ultrasound-diagnosed synovitis was also shown to be associated at baseline with joint erosions on x-ray.
The researchers confirmed that synovitis on ultrasound provided value in predicting RA flare (as defined by the patients' Disease Activity Score and flare questionnaires at six months of follow-up). However, they also found that tenosynovitis on ultrasound was associated with flare more specifically, as defined by exacerbation of symptoms and the resulting need to increase therapy.
| Association of US factors with RA flare, by odds ratio | |||
| US factors | Elevated Disease Activity Score | Need to increase therapy | Patient-reported flare on questionnaire |
| Positive power Doppler US for tenosynovitis | 0.98 | 1.68 | 1.08 |
| Positive grayscale US for tenosynovitis | 1.21 | 1.87 | 0.75 |
| Positive power Doppler US for synovitis | 2.01 | 1.02 | 1.58 |
| Positive grayscale US for synovitis | 1.81 | 1.51 | 0.54 |
Bellis noted that the study is still ongoing: The preliminary results are from the first six months of the yearlong follow-up. She also acknowledged several limitations of the project, including its reliance on static ultrasound images, the heterogeneity of the ultrasound scanners used in the study, and underpowered statistical analyses.
Subclinical synovitis
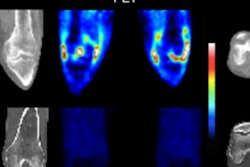
In the second study presented at EULAR 2015, the team from Japan wanted to determine if RA patients in remission but with subclinical synovitis should be treated more intensively. RA patients in clinical remission may still have progression of joint damage, and power Doppler ultrasound can show subclinical synovitis, according to presenter Dr. Tadashi Okano of Osaka University.
For the prospective randomized controlled trial, the researchers enrolled 134 RA patients who were in clinical remission between June 2012 and April 2013. All patients in the study were 20 years or older, had been in clinical remission continuously for the past three months, and had received stable treatment for the past three months. The researchers did not include patients who had contraindications to methotrexate (MTX) therapy or who had other overlapping rheumatic diseases.
Ultrasound was performed using a Hi Vision Avius system (Hitachi Aloka Medical) with a 6- to 14-MHz broadband linear probe. Thirty-four synovial sites in 30 joints were scanned, including the first to fifth metacarpophalangeal joints, the first interphalangeal joint, and the second to fifth proximal interphalangeal joints in the hand. The radial, median, and ulnar aspects of the wrist were also scanned, as well as the second to fifth metatarsophalangeal joints of the foot.
Several scoring methods were used, including semiquantitative assessment on grayscale and power Doppler, a global index for grayscale synovial hypertrophy, and a global index for synovial power Doppler signal.
Of the 134 patients who received a baseline ultrasound exam, 101 (75.4%) had positive power Doppler ultrasound exams for active synovitis and 33 did not. Those with positive scans were randomized into two groups: an intensive treatment group (50 cases) that received an increased dose of MTX and a continuous treatment group (51 cases) that continued with the current level of treatment.
Follow-up was performed over a year; clinical assessment, ultrasound, and x-ray exams were performed at baseline, week 24, and week 52. The study's primary end point was change in radiographic joint damage as determined via the modified total Sharp score (mTSS) method for measuring arthritis progression.
Due to factors such as patients discontinuing participation in the study and protocol violations, yearlong follow-up was available for 42 patients in the continuous treatment group and 37 patients in the intensive treatment group. It was also available for 20 of the patients who did not have synovitis on power Doppler ultrasound.
The researchers found that the intensive treatment had a significant effect, as indicated by total mTSS score (the lower the score, the less the arthritis progressed).
| Effectiveness of therapy, by total mTSS score | |||
| Time point | Group that received continuous therapy | Group that received intensive treatment | p-value |
| Week 24 | 1.02 | 0.27 | 0.007 |
| Week 52 | 2.02 | 1.03 | 0.038 |
"Subclinical active synovitis in clinical remission patients was decreased by additional intensive treatment," Okano said. "This resulted in the prevention of ... joint damage progression even in remission patients."
Dose escalation of MTX was difficult in some patients due to nausea or liver dysfunction, the researchers noted.
"Other options, such as articular injection of glucocorticoid, should be considered for additional intensive treatment," Okano said.