Digital breast tomosynthesis (DBT) is superior to full-field digital mammography (FFDM) for detection of microcalcifications, according to an Italian researcher, who believes the study marks another step toward the evolution of more routine use of 3D mammography in breast imaging.
Microcalcifications are a common finding in the breast, and they may represent an early sign of breast cancer, in particular, ductal carcinoma in situ (DCIS), said Dr. Paola Clauser at last month's ECR 2015. While FFDM performs well for microcalcifications, DBT might be even better.
Prior to studying how DBT compares with FFDM, researchers have said, "FFDM is the best imaging modality that we have to detect and characterize this type of microcalcification," according to Clauser, who is finishing her residency at the University of Udine in Italy.
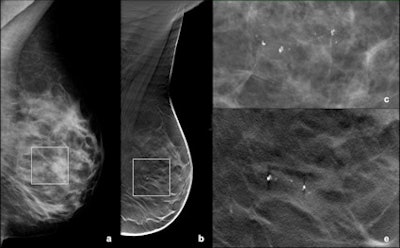
![A small cluster of heterogeneous microcalcifications was visible on FFDM (a: mediolateral oblique [MLO] view; c: particular digitally magnified) in the central, prepectoral, area of the right breast. The finding was clearly visible on DBT (b: MLO view; e, f: particular digitally magnified), and in both imaging modalities was classified as suspicious. The patient underwent vacuum-assisted biopsy and histology was intermediate grade DCIS. All images courtesy of Dr. Paola Clauser.](https://img.auntminnieeurope.com/files/base/smg/all/image/2015/04/ame.2015_04_30_09_21_35_578_2015_04_30_dbt_calcifications_pic1.png?auto=format%2Ccompress&fit=max&q=70&w=400) A small cluster of heterogeneous microcalcifications was visible on FFDM (a: mediolateral oblique [MLO] view; c: particular digitally magnified) in the central, prepectoral, area of the right breast. The finding was clearly visible on DBT (b: MLO view; e, f: particular digitally magnified), and in both imaging modalities was classified as suspicious. The patient underwent vacuum-assisted biopsy and histology was intermediate grade DCIS. All images courtesy of Dr. Paola Clauser.
A small cluster of heterogeneous microcalcifications was visible on FFDM (a: mediolateral oblique [MLO] view; c: particular digitally magnified) in the central, prepectoral, area of the right breast. The finding was clearly visible on DBT (b: MLO view; e, f: particular digitally magnified), and in both imaging modalities was classified as suspicious. The patient underwent vacuum-assisted biopsy and histology was intermediate grade DCIS. All images courtesy of Dr. Paola Clauser.Most studies show DBT has a good performance on masses and helps with asymmetries, but there isn't much research on calcifications and microcalcifications, she said.
"There are just a few published studies and the results are not exactly completely concordant," she added. "Some say that DBT is very good, some others say we need more help and we still need a lot of digital mammography. So, we decided to assess the value of DBT for the detection and the characterization of microcalcifications as compared to FFDM."
Collaboration with Vienna
During a research fellowship at the Medical University of Vienna, Clauser and colleagues conducted a study involving 150 consecutive patients. They retrospectively selected 50 negative BI-RADS 1 cases with at least 1-2 years follow-up, and 50 positive cases, all proved by histology. They also included 50 benign cases of microcalcifications and 50 cases of malignant microcalcifications.
All patients underwent FFDM (Mammomat Inspiration, Siemens Healthcare,) and DBT (also Mammomat Inspiration). The scan angle for DBT was 50° with 25 projections, and filtered back projection (FBP) data reconstruction was used. All imaging data were reviewed by four readers independently. The readers were divided into experienced (read a total of more than 1,400 DBT exams) and inexperienced. Image analysis included the presence of calcifications, breast density, BI-RADS calcification descriptors (distribution and morphology), visibility in both views, conspicuity of calcifications, and assignment of a final BI-RADS assessment category.
 A small group of amorphous microcalcifications was detected in the retro-areolar region of the left breast with both FFDM (a: MLO view; c: particular digitally magnified) and DBT (b: MLO view; d: particular digitally magnified). Vacuum-assisted biopsy was performed and histology showed fibrocystic changes.
A small group of amorphous microcalcifications was detected in the retro-areolar region of the left breast with both FFDM (a: MLO view; c: particular digitally magnified) and DBT (b: MLO view; d: particular digitally magnified). Vacuum-assisted biopsy was performed and histology showed fibrocystic changes.DBT's sensitivity for calcification detection was 94.5%, which was superior to FFDM at 92.5%. There was no statistically significant difference in the area under the curve (AUC) of BI-RADS assessment categories for DBT (0.833) and FFDM (0.829). One reader found a statistically significant higher visibility for calcifications in DBT (AUC = 0.63, p = 0.002). The other readers found the conspicuity of DBT and FFDM were similar. Inter-reader agreement of DBT and FFDM was 0.356-0.494 for distribution, 0.240-0.383 for morphology, and 0.498-0.546 for breast density and comparable for both modalities.
When expert readers were compared with nonexpert readers, nonexpert readers had a significantly higher sensitivity, but expert readers had a significantly higher specificity in the characterization of microcalcifications, noted Clauser et al.
| DBT sensitivity and specificity for expert vs. nonexpert readers | ||
| Sensitivity | Specificity | |
| Expert reader 1 | 78% | 78% |
| Expert reader 2 | 86% | 67% |
| Nonexpert reader 1 | 98% | 54% |
| Nonexpert reader 2 | 88% | 59% |
However, when the AUC was examined, there was no significant difference in reader performance, either with the modality or between readers with different experience, so overall the performance with DBT and digital mammography was very good, irrespective of readers' experience.
"We found significant difference in readers' sensitivity and specificity according to their experience with DBT," Clauser said in an interview with AuntMinnieEurope.com. "As in FFDM, microcalcifications are difficult to properly assess, and training is needed, more for microcalcifications than for soft-tissue lesions that, as a general rule, appear more clearly and can be more easily classified with DBT as compared to FFDM."
Clauser believes the results represent another step in the evolution of breast cancer care.
"Most likely, we will not be able to avoid 2D images any time soon, but it is likely that synthetic 2D images will be more than enough to interpret an examination, even for microcalcifications, without the need for a proper FFDM," she said. "Though we did not address directly the issue of acquisition parameters, it is interesting to notice that our results were obtained with a DBT that uses a wide angle for image acquisition, which according to the literature, is not the best to visualize microcalcifications. Thus, we do believe these results could be at least confirmed when using other devices available."
Considering the confidence intervals, DBT performs equally to FFDM.
"[T]his is important as our evaluation confirms that we can also use DBT for assessment of microcalcifications," she said. "Before, we regularly concentrated on mammograms only. Further, we have to some amount reduced the number of additional magnification views in our clinical practice. I think we can safely say that we are more confident in gathering information from the 3D images for all lesions, also calcifications. However, it is too soon to say whether or not we can generally avoid magnification views."
As for future research, Clauser et al are analyzing whether 3D assessment using DBT improves the assessment of microcalcification morphology. An improved characterization might improve specificity of microcalcification assessment, she said.



















