Groundbreaking research about MRI's expanding role in the planning, safety, evaluation, and success of uterine artery embolization won a Portuguese group a prestigious Magna Cum Laude award at this month's ECR 2015 in Vienna.
With MR angiography (MRA), MRI is an invaluable tool in patient selection, appropriate patient counseling, angiographic procedure planning, evaluation of technical effectiveness of the treatment, and identifying most postembolization complications. It is vital to the outcome of uterine artery embolization (UAE), explained Dr. Cristina Maciel and colleagues from the department of radiology at Hospital de São João in Porto.
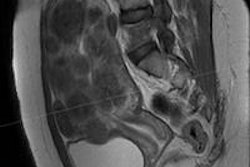
Before a procedure, MRI helps confirm the diagnosis of uterine fibroids and detect coexisting adenomyosis. Large fibroid size and submucosal component can result in postembolization complications and may affect the decision to offer UAE. Patients with fibroids that have already infarcted are unlikely to show improvement of symptoms with UAE, while embolization of pedunculated subserosal fibroids is not associated with additional complications, they stated in their award-winning e-poster.
 The range of materials used during a uterine fibroid embolization procedure. Photo courtesy of Dr. Jamal Al Koteesh.
The range of materials used during a uterine fibroid embolization procedure. Photo courtesy of Dr. Jamal Al Koteesh."MR angiography provides useful information to the interventionist, namely the 3D configuration of the uterine arteries, the presence of enlarged ovarian arteries, and identification of the optimal tube angle for angiographic selection of the uterine arteries, thus improving operative performance of UAE," the authors noted.
Postprocedural MRI can evaluate the technical effectiveness of the treatment -- ideally complete devascularization and shrinkage of fibroids -- and can identify postembolization complications.
It is important to be aware of the MRI features of the most common coexisting conditions and alternative diagnosis to uterine fibroids, as well as the relevant MRI findings that may influence the planning of UAE, i.e., the location, size, and enhancement of fibroids. Keep in mind the merits of performing MRA of the pelvic vasculature prior to UAE, with the emphasis on variant pelvic arterial anatomy relevant to perform UAE. MRI assessment after UAE, including evaluation of fibroid infarction, changes in fibroid size and location, fibroid regrowth and recurrence, is also important, they continued.
"There is emerging evidence for the use of MRA for planning and improving operative performance of UAE. MRA allows pretreatment assessment of the normal and variant pelvic arterial anatomy. Additionally, MRA may depict enlarged ovarian arteries possibly supplying uterine fibroids," Maciel et al stated. "MRA is also useful in the prediction of the optimal projection angle to demonstrate uterine artery origin at subsequent angiography, reducing radiation dose, fluoroscopy time, and volume of contrast medium used."
Adenomyosis, endometriosis, solid adnexal masses, myometrial contractions, musculoskeletal and genitourinary pathology, and occasionally uterine leiomyosarcomas may be incidental MRI findings, and they may provide an alternative explanation for the patient's symptoms. Some of these conditions may preclude UAE or influence the outcome.
Adenomyosis is the intrauterine counterpart to endometriosis, and can be focal or diffuse, and occasionally it mimics fibroids, although the two conditions may coexist.
"Unlike fibroids, adenomyosis generally lacks distinct margins and exerts no mass effect. Instead of displacing or distorting the adjacent endometrium, adenomiosis abuts the endometrium without displacement. Adenomyosis signal intensity approximates junctional zone hypointensity with possible intralesional T1 and/or T2 hyperintensities," the authors wrote. "A junctional zone measurement of 12 mm or greater confirms the diagnosis of adenomyosis; between 8 and 12 mm is indeterminate."
Coexistent adenomyosis should be noted before performing UAE, and patients should be informed of a more variable outcome, they added.
The differential diagnosis between pedunculated fibroids and solid adnexal masses can be challenging whenever normal ovaries are not clearly depicted. Ovarian fibromas and Brenner tumors are benign ovarian neoplasms that have a large fibrous component and can have signal intensity similar to that of a pedunculated fibroid. MRI can show fibromas and Brenner tumors surrounded by ovarian stroma and follicles, establishing the ovarian origin of the mass and allowing exclusion of a diagnosis of fibroid. If the bridging vessel sign is present, the diagnosis of fibroid is possible, as continuity of the mass with the adjacent myometrium is demonstrated.
Complex masses suspicious for ovarian malignancy need to be diagnosed before UAE, and the presence of benign ovarian masses is not a contraindication to UAE, according to the researchers.
Myometrial contractions may simulate a fibroid (or focal adenomyosis) on MRI, and can appear as transient hypointense T2-weighted masses. The key to this diagnosis is changeability, and each sequence should be checked for interval change or resolution to confirm a myometrial contraction.
Diagnosis of uterine leiomyosarcoma (LMS) in the absence of metastatic disease remains difficult, they explained. Rapid growth is often suggestive of LMS, and continued growth after embolization is an important sign of possible malignancy. Imaging features that should generally raise concern for LMS include a large mass with a bizarre appearance that includes marked cystic-appearing changes and areas of high signal on T1-weighted imaging resulting from hemorrhage. These imaging appearances should prompt consideration of surgical management, biopsy before UAE, or short-interval follow-up imaging; known or suspected gynecologic malignancy is an absolute contraindication to UAE.
In most cases where LMS is in the differential diagnosis, histologic diagnosis tends to reveal a benign fibroid.
Copper-containing intrauterine devices (Cu-IUD) are MR-safe for women scanned on a 1.5-tesla system. Some models of Cu-IUD are classified as MR conditional and do not pose known hazards, provided that the MRI is of a maximum of 3-tesla. Presence of an IUD/IUS is not considered a contraindication for UAE. Detailed information can be found on www.MRIsafety.com.
"Many interventionists maintain a threshold for embolization of 13-15 cm for the longest fibroid axis. Above this, the postembolization volume may still result in bulk symptoms, and the necrosis from a large fibroid may result in a prolonged postembolization syndrome," the authors continued.
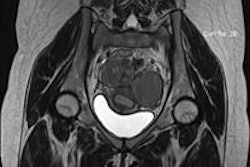
Enhancement of fibroids depends on their vascularity. Gadolinium-enhanced T1-weighted fat-saturated sequences are essential to demonstrating fibroid vascularity. Vascularity varies and enhancement ranges from virtually absent (avascular) to marked enhancement (hypervascular) compared with the adjacent myometrium.
Cellular leiomyomas, comprising compact smooth muscles cells with little or no collagen, can have relatively increased T2-weighted signal intensity and tend to have marked homogeneous enhancement on contrast-enhanced images. Fibroids that have already infarcted are unlikely to show volume reduction with UAE, and therefore improvement of symptoms is less likely.
Fibroids with high T2 signal and gadolinium enhancement tend to respond better to UAE, whereas fibroids with increased T1 signal and less gadolinium uptake may not shrink significantly following UAE. Persistent enhancement of fibroids after UAE is a sign of treatment failure that may need additional treatment including repeated UAE or surgery. Although all fibroid locations are eligible for embolization, certain anatomic fibroid subtypes deserve special consideration, they believe.
"Although conventional angiography remains the gold standard for arterial visualization, MRA may help the interventionist to obtain a better understanding of the arterial anatomy before UAE," Maciel et al wrote. "Also, knowledge about the presence of ovarian artery collateral supply to the fibroid before performing UAE is important for planning UAE as well as for selecting and counseling the patients, because ovarian artery embolization itself may result in ovarian dysfunction."
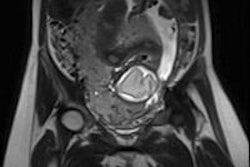
Fibroid calcification typically occurs six months after UAE, and can be peripheral or central. On MRI, the calcifications appear as areas of low signal on all sequences.
The goal of UAE is 100% infarction of uterine fibroids to achieve optimal and extended improvement in preprocedure symptoms, they noted. Residual viable leiomyoma tissue may result in failure of UAE due to regrowth of uterine fibroids. Fibroid recurrence after UAE can occur due to newly developed fibroids tumor and/or to regrowth after incomplete embolization. Fibroid recurrence is a problem also seen with myomectomy and other uterine-sparing therapies.
Transcervical expulsion of a fibroid/fibroid tissue is one of the more common complications after UAE occurring in about 5% of patients and in some requiring surgical extraction. Submucosal fibroids, intramural fibroids in contact with the endometrial surface, and intracavitary fibroids are at increased risk for transcervical expulsion. MRI is the first-line modality in evaluating for suspected sloughing/expulsion of a fibroid, the authors concluded.