The holy grail of diagnostic imaging is noninvasive tissue characterization and the external identification of human cell structures and organ function, if possible without even touching the body. Magnetic resonance was meant to bring this most sought-after achievement in medical diagnostics: T1 and T2 relaxation times were to be the key to it.
The use of relaxation times for medical applications was introduced in 1955/1956 by Erik Odeblad and Gunnar Lindström. Since then, this idea has occupied the minds of many researchers. Nearly 20 years after Odeblad's description, a New York physician, Raymond Damadian, patented a method for relaxation time measurements in malignant diseases. Unfortunately for him and for mankind, it didn't work.
 Dr. Peter Rinck, PhD, is a professor of diagnostic imaging and the president of the Council of the Round Table Foundation (TRTF) and European Magnetic Resonance Forum (EMRF).
Dr. Peter Rinck, PhD, is a professor of diagnostic imaging and the president of the Council of the Round Table Foundation (TRTF) and European Magnetic Resonance Forum (EMRF).What is T1 and which factors are influencing it? T1 depends on several parameters, among them the resonance frequency (field strength), temperature, microviscosity of observed spins, presence of large molecules, and presence of paramagnetic ions or molecules. The precise calculation of true T1 and T2 values is extremely complex and in vivo almost impossible.
When we started creating synthetic images based on the three main contrast parameters in MRI, viz. T1, T2, and proton density, in the early 1980s1 and the image simulation software "MR Image Expert" some years later, these parameters were based on time-consuming, but precise data acquisitions and exact calculations. They allowed the creation of outstandingly good simulations of MR images -- but still simulations. More details can be found in textbooks, for instance online at "Magnetic Resonance in Medicine".2
Researchers have left no stone unturned: In vivo relaxation time measurements based on MR imaging have been tried out over the years by a large number of people, who have measured relaxation time values for tissue characterization in the brain and all over the body, including muscles and bones. The task proved to be in vain because all efforts to characterize or even type tissue largely failed.
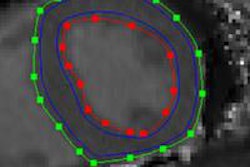
The reasons are manifold and include systematic measurement errors, inaccuracy of plotting methods of relaxation curves, inherent variability of tissue composition, partial volume effects, and interobserver variability. Researchers realized that it is futile to measure a point or a region of interest because too many different components such as tumor, fat, fibrotic or necrotic cells, small vessels, calcifications, and other structures can be found within a volume of interest. In addition, T1 and T2 values of diseased cells overlap with those of other pathologies, edema, and sometimes normal tissue: T1 and T2 of normal tissue change with age and hormonal cycles, breast tissue being a good example.
When absolute T1 or T2 values were finally deemed not leading anywhere, combinations of T1 and T2, histogram techniques, and more sophisticated 3D display techniques of factor representations were applied. However, the heterogeneity of normal tissues as well as of pathological benign and malignant tissues did not allow the pathologist's view through the microscope to be replaced with MR techniques.
After more than 30 years of unsuccessful trials, the cardiologists arrived. They would like to distinguish fibrotic, inflammatory, and infiltrative cardiomyopathies, myocardial edema, as well as normal myocardium from each other and quantitatively diagnose myocardial fibrosis.
Because the acquisition of quantitative tissue data from a beating heart has to be very fast, they rely on a modified pulsed NMR sequence proposed by David C. Look and Donald R. Locker in 1969. MRI did not exist at that time, and Look and Locker used their time-saving one-shot method for NMR spectroscopy instead of the conventional methods to measure the T1 relaxation time. The spectroscopic "LL" method was within 10% of the conventionally calculated value.3
In the 1980s, the method was further developed for MRI by Graumann and his colleagues.4 Others followed. The modified sequences for cardiac MRI used today are called MOLLI5 and ShMOLLI6; some different pulse sequences, e.g., SASHA and SAPPHIRE are also being tested.
The support is enthusiastic, several thousand papers were published during the last ten years and approximately 150 patents were applied for.
Most cardiac T1 papers are based on mathematical simulations and hypotheses or speculations. Although in many publications there is a lot of talk about accuracy and precision, a major problem of MOLLI and ShMOLLI is their inaccuracy and their errors. The MOLLI scheme does not calculate true T1 but apparent T1 values for which a new, nonfitting name was invented: T1* (T-one star). In review papers7, 8 more pages are filled with explanations of errors, euphemistically dubbed "confounders," than about real measurements and comparative results. Just reading these papers clarifies the futility of the method.
Many researchers seem not to be scientifically literate -- lacking understanding of basic and established principles of physics and engineering. Far away from solid magnetic resonance science, mainstream cardiac MR research seems to develop into a kind of pseudoscience aiming at rather vague T1* MOLLI numbers. If the values measured cannot be reproduced on different days or on different machines of the same model, they are useless for science and medicine. Still, there are no comparative studies of such sequences and true T1 and T2 measurements. Instead, the developers and researchers continue to discuss infinitesimal refinements and modifications of their sequences.
At a meeting in January, Robert N. Muller, professor emeritus of the University of Mons and former head of one of the world's most prestigious centers for NMR relaxometry and MRI contrast agent design, dismissed the studies as scientifically without foundation and stated: "If you don't measure T1, you cannot talk about T1-mapping. It measures MOLLI time and is MOLLI-mapping. If you can't be precise from the onset, don't continue."
Even measurements of true T1 and T2 relaxation times allow only global statements but no clear tissue characterization or grading.
From dernier cri of cardiological technology to déjà vu of recurrent failure of T1-mapping is a short step.
Where is the value or added value for research and patients? I don't see any. Churning up and out numbers is meaningless. There is a wide range of "normal" values, the range of normal myocardium at 3-tesla stretches from 1,000 to 1,300 ms; but hardly any "apparent T1 values" of pathologies were published.
It is foreseeable that measurements of pathologies will overlap with each other and those of with normal tissue. One cannot trust these numbers. However, the clinicians just seem to be in awe of the pulse sequence researchers -- because they don't understand anything; most of them lack the background in pulse sequence design, biochemistry, or metabolism.
I found the following well-fitting statement in a recent editorial of a cardiology journal: "Cardiology journal editors have adopted a laudable policy of intentionally reporting negative studies in humans, viewing these negative results as important contributions to the understanding of the field. This may very well include high-ranked journals such as the JACC or the EHJ."9
However, one should also try to find some research that contributes to the positive furtherance of cardiology (and radiology).
Note: This article uses some text passages I published more than 20 years ago in Radiology and elsewhere. Not much has changed since.10
Dr. Peter Rinck, PhD, is a professor of diagnostic imaging and the president of the Council of the Round Table Foundation (TRTF) and European Magnetic Resonance Forum (EMRF).
References
- Bielke G, Meves M, Meindl S, et al. A systematic approach to optimization of pulse sequences in NMR-imaging by computer simulations. In: Esser PD, Johnston RE, eds. The Technology of NMR. New York: The Society of Nuclear Medicine Computer and Instrumentation Councils; 1984:109-117.
- Rinck PA. Magnetic Resonance in Medicine. The Basic Textbook of the European Magnetic Resonance Forum. 8th ed.; 2014. http://magnetic-resonance.org/ch/04-06.html.
- Look DC, Locker Dr. Pulsed NMR by tone-burst generation. J Chem Phys. 1969;50:2269-2270.
- Graumann R, Barfuss H, Fischer H, Hentschel D, Oppelt A. TOMROP: A sequence for determining the longitudinal relaxation time T1 in magnetic resonance tomography. Electromedica. 1987;55:67-72.
- Messroghli DR, Radjenovic A, Kozerke S, Higgins DM, Sivananthan MU, Ridgway JP. Modi?ed Look-Locker inversion recovery (MOLLI) for high-resolution T1 mapping of the heart. Magn Reson Med 2004;52(1):141-146.
- Piechnik SK, Ferreira VM, Dall'Armellina E, et al. Shortened modified Look-Locker inversion recovery (ShMOLLI) for clinical myocardial T1-mapping at 1.5 and 3 T within a 9 heartbeat breathhold. J Cardiovasc Magn Reson. 2010;12:69.
- Kellman P, Hansen MS. T1-mapping in the heart: Accuracy and precision. J Cardiovasc Magn Reson. 2014;16:2.
- Perea RJ, Ortiz-Perez JT, Sole M, et al. T1 mapping: Characterisation of myocardial interstitial space. Insights Imaging. 2014 Nov. 26 epub ahead of print.
- Atar D, Agewall S. End of story? Studies on prevention of reperfusion injury encounter perpetual defeats. European Heart Journal -- Cardiovascular Pharmacotherapy. 2015; 1:46-47.
- Rinck PA, Fischer HW, Vander Elst L, Van Haverbeke Y, Muller RN: Field cycling relaxometry: Medical applications. Radiology. 1988;168:843-849. Review paper: Rinck PA: The clinical utility of the measurement of T1 and T2 in whole body MRI. In: Grant DM and Harris RK, eds. Encyclopedia of Nuclear Magnetic Resonance. John Wiley and Sons: Chichester; 1996: 4042-4045.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnieEurope.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.