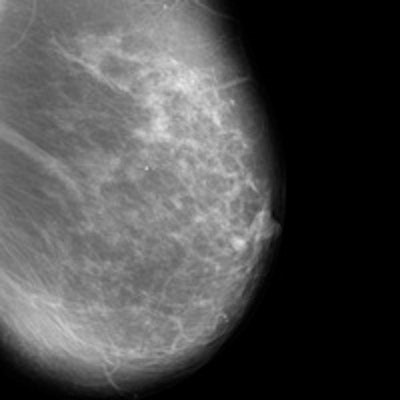
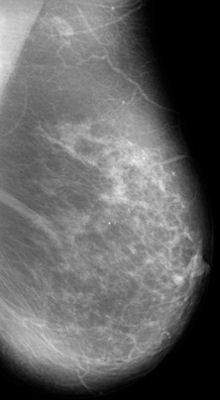
In a new 16-year study, Spanish researchers have found that switching to full-field digital mammography (FFDM) leads to early diagnosis, not overdiagnosis. The group found that cancer detection rates did not increase when compared with film-screen mammography, but going digital did lead to an increase in ductal carcinoma in situ (DCIS) detection rates.
Some observers fear that switching to FFDM increases the negative effects of screening through overdiagnosis, or the detection of cancers that may not pose a health hazard to patients in their lifetime. The new research shows, however, that DCIS detection is higher with FFDM than with analog mammography, and there is also a trend to identify less advanced invasive cancers. The results mean two things: either there's an improvement in early diagnosis with FFDM, or there's an increase in overdiagnosis.
To test these hypotheses, researchers decided to examine indicators of the performance of breast screening, including interval cancer, sensitivity, specificity, positive predictive value, and tumor characteristics, according to Dr. Maria Sala from the epidemiology and evaluation department at Hospital del Mar Medical Research Institute in Barcelona, Spain, and colleagues in an article published online by European Radiology (September 26, 2014).
One of the study's strengths is its length: It covers 16 years of breast screening, six of which with digital mammography.
"Most of the studies provide data only from the first one or two screening rounds performed with FFDM, which may have been influenced by the transition from one technology to the other, as well as by the learning curve," they wrote. "Therefore, the evolution of quality indicators in subsequent digital screening rounds has scarcely been evaluated. Evaluation of the long-term effect of FFDM on the screening performance indicators within a cohort perspective is required for a complete evaluation of screening."
The researchers included 82,961 film-screen and 79,031 FFDM studies acquired in women ages 50 to 69 who were screened biennially from 1995 to 2010 in Spain and followed up to 2012. Rates of cancer detection, interval cancer, tumor characteristics, and other quality indicators were compared between the analog and digital periods.
They found that sensitivity of both approaches was similar: 75.16% for SFM and 75.17% for FFDM, while specificity was 95.19% for analog mammography and 96.60% for digital. The positive predictive value (PPV) was 8% for film-screen and 11.25% for digital mammography. Other performance indicators are as follows:
| Performance of film-screen mammography vs. FFDM | ||
| Film-screen | FFDM | |
| DCIS rate | 0.05% | 0.09% |
| False-positive rate | 4.79% | 3.38% |
| Cancer detection rate | 0.42% | 0.43% |
| Interval cancer rate | 0.14% | 0.14% |
| Recall rate | 5.57% | 4.2% |
The results were expected and desirable, Sala wrote in an email to AuntMinnieEurope.com. "After two studies in our context showing the lower recall rate and false-positive results after the introduction of digital mammography, we had to confirm that we did not have an increase of interval cancers. And, at the same time, we wanted to better understand the increase of DCIS."
The findings points to a stage shift, especially when analyzing the size of invasive tumors -- the proportion of smaller invasive tumors tended to increase during the FFDM periods. Also, the proportion of high-grade DCIS was higher but not statistically significant.
The proportion of high-grade DCIS detected is higher with FFDM because of early diagnosis, she explained.
"We detect more high-grade DCIS (which would have become invasive tumors later) and smaller invasive cancers," she wrote in her email. "It has been demonstrated that high-grade DCIS are precursor of invasive cancers. On the contrary, low-grade DCIS have not been demonstrated to be a precursor form of invasive cancers, and some authors have related them with nonprogression and overdiagnosis."
In the study, Sala and colleagues wrote that because low-grade DCIS may have a lower potential to become invasive, the similar proportions observed in the two periods do not support the hypothesis of overdiagnosis. However, larger series are necessary to confirm this trend.
The researchers concluded that the increase in DCIS detection is partly due to an improvement in early diagnosis and confirms the reduction in the false-positive rate with no increase in the interval cancer rate.
"In view of the current results, which are supported by those from previous studies performed in different countries, the use of digital technology should not be seen as a threat that increases the negative effects of screening through overdiagnosis," they wrote. "Future recommendations on screening performance and quality standards should be updated with information from screening settings using this technology."



















