A breast screening protocol that combines single-view digital breast tomosynthesis (DBT) with single-view 2D digital mammography (DM) had higher sensitivity for detecting breast cancer than two-view 2D digital mammography, with just a slight increase in radiation dose, according to a new study in European Radiology.
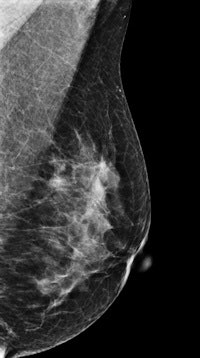
South Korean researchers also discovered that the differences in radiation dose between the two techniques varied based on the density and thickness of breast tissue, with the variance lowest in women with dense and thick breasts. This finding indicates that breast imagers could fine-tune which women receive DBT and which are sent for 2D mammography (Eur Radiol, 3 September 2014).
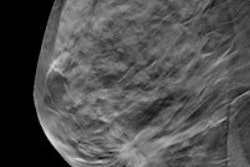
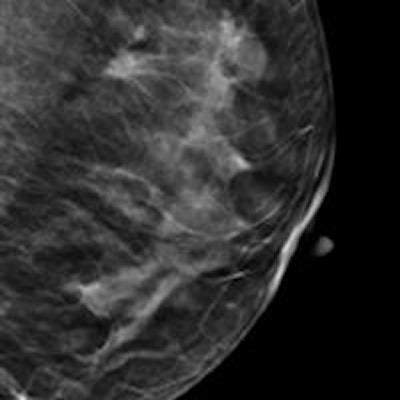
DBT has been gaining popularity with the publication of studies indicating that it has a higher cancer detection rate and lower recall rate compared with 2D mammography, particularly in women with dense breast tissue. But many of these studies have used two-view DBT protocols that acquire both mediolateral oblique (MLO) and craniocaudal (CC) views -- and this can create issues regarding radiation dose and length of reading time.
As an alternative, researchers have developed techniques that combine single-view DBT with single-view 2D mammography and have reported good performance for this combined protocol compared with two-view 2D digital mammography. But no study has reported on both diagnostic performance of the combined protocol and its radiation dose, according to Dr. Sung Ui Shin from the radiology department at Seoul National University Hospital and colleagues.
The researchers decided to do just that in a retrospective study involving 149 patients using a commercially available tomosynthesis system (Selenia Dimensions, Hologic). Of the group, 102 patients (68.5%) had malignancies, while 47 individuals (31.5%) were considered to have negative or benign findings.
The combined technique used an MLO DBT view combined with a CC 2D digital mammography view. Three readers reviewed all studies and calculated their specificities and sensitivities. The data were also analyzed by breast thickness and density, while radiation dose for both techniques was represented by average glandular dose (AGD).
When combining the results of the three readers, the researchers found a mean sensitivity advantage for the combined technique that was statistically significant (p < 0.001), while the mean specificity difference did not reach statistical significance (p = 0.26). Radiation dose was slightly higher for the combined technique.
| Single-view DBT + 2D mammography vs. two-view 2D mammography | |||
| Single-view DBT + 2D DM | Two-view 2D DM | ||
| Mean sensitivity | 89.5% | 82.4% | |
| Mean specificity | 78.5%* | 75.1%* | |
| Mean average glandular dose | 1.74 mGy | 1.63 mGy | |
When further analyzing radiation dose, the researchers found that the difference between the combined protocol and two-view 2D digital mammography varied based on the type and thickness of breast tissue. In essence, breast thickness and density were independent factors associated with AGD difference, and the difference was significantly smaller in dense and thick breasts than in fatty and thin breasts.
"Our results show that the clinical benefit in using the combined technique of single-view DBT and single-view DM not only improves diagnostic performance but also minimizes radiation dose increments in patients with dense breasts," the authors wrote. "Thus, for dense- or thick-breast patients, we can expect higher diagnostic performance with a small dose difference using MLO DBT instead of MLO DM."
Other study limitations include its retrospective nature; the reader studies were enriched with malignant lesions and, thus, the results may be different from a true screening population; the number of patients with fatty breasts was relatively small; images were obtained on a clinically proven platform with established techniques, and dose values retrieved from the DICOM header were not verified; and prior imaging studies were not available to the readers in helping them make assessments.
Although the mean radiation dose of the combined DBT plus DM protocol was slightly higher than two-view digital mammography, the difference in dose was lower for patients with dense breasts, meaning that the protocol could be particularly useful for these individuals, the researchers concluded.
"Particularly in dense breast patients, single-view MLO DBT plus single-view CC DM may provide better diagnostic performance with a minimal increase in AGD," they wrote.