
Patients with suspected idiopathic pulmonary fibrosis (IPF) who do not have typical patterns on high-resolution CT (HRCT) may in the future be spared the risks of lung biopsy and be given a confident diagnosis based on clinical and radiological findings alone, according to new research published in Lancet Respiratory Medicine.
In a retrospective study of 315 patients who were 40 years old and older and having little or no (5% or less) honeycombing on HRCT, 79 (94%) of the 84 patients who had a high-resolution pattern of possible usual interstitial pneumonia (UIP) diagnosed by an expert radiologist and pathologist had histopathological UIP confirmed after analysis of lung biopsy samples (Lancet Respir Med, 18 February 2014).
"Our findings suggest that when a team of multidisciplinary experts in interstitial lung disease at a regional center (that includes a chest radiologist and a pulmonologist) work together to interpret possible UIP pattern on high-resolution CT in a patient suspected to have IPF, surgical lung biopsy might not be necessary to reach a diagnosis of IPF," noted lead author Dr. Ganesh Raghu, professor of medicine in the Division of Pulmonary and Critical Care Medicine at the University of Washington Medical Center in Seattle, and colleagues.
','dvPres', 'clsTopBtn', 'true' );" >
Click image to enlarge.
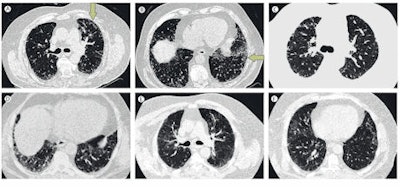
High-resolution axial CT images of upper and lower lung. A-B: Usual interstitial pneumonia; images show peripheral predominant, basal predominant reticular abnormality with mild subpleural honeycombing (B, arrows). The extent of honeycombing is < 5%. C-D: Possible usual interstitial pneumonia; images show peripheral predominant, basal predominant reticular abnormality without honeycombing. E-F: Inconsistent pattern of usual interstitial pneumonia; images show upper lung predominant abnormality characterized by ground glass abnormality with mild reticular abnormality. Images courtesy of Dr. Ganesh Raghu, reproduced with permission from the Lancet Respiratory Medicine.
The results will also help to provide clarity about treatment options for a greater number of patients and increase the pool of patients suitable for inclusion in clinical trials of new therapies, according to Simon Hart, PhD, senior lecturer in respiratory medicine at Hull York Medical School in the U.K.
"In the modern era with optimal high-resolution CT imaging and thoracic radiologists familiar with interpretation of interstitial lung disease patterns through participation in multidisciplinary meetings, the role of lung biopsy assessment might diminish further," he wrote in a linked editorial. "In future, the combination of high-resolution CT with new noninvasive biomarkers and functional imaging could be used to better define phenotypes of fibrotic interstitial lung disease."
HRCT scans of the lungs can identify typical "honeycombing pattern" of lung scarring and damage to the air sacs known as UIP in patients with IPF, explained Raghu et al. In a patient with progressive breathlessness who has no significant environmental exposures attributable to pulmonary fibrosis, or evidence of collagen vascular diseases, the UIP pattern on HRCT is characteristic of IPF. When patients suspected of having IPF do not have the definitive UIP pattern on HRCT images, international guidelines recommend a surgical lung biopsy to make a confident diagnosis of IPF in such cases.
"Surgical lung biopsy is associated with substantial risks and many patients are too elderly, sick, and/or have comorbid conditions to tolerate the invasive procedure," they stated.
IPF causes progressive scarring of lung tissue, which eventually prevents the lungs from being able to supply the body with adequate oxygen. It has no cure, and most patients live only three to five years after diagnosis. Appropriate treatment is complicated by the fact that a definitive diagnosis often requires a lung biopsy. Furthermore, studies from the U.K. and U.S. suggest IPF is becoming more common.
There are an estimated 5,000 new cases in the U.K. each year, and IPF causes more deaths each year than leukemia, ovarian cancer, or kidney cancer. In the U.S., about 50,000 new cases are diagnosed each year, and as many as 40,000 U.S. patients die from IPF each year, the same number as who die from breast cancer.
"A confident diagnosis of IPF is needed to ensure that patients are well informed of the poor prognosis associated with IPF, are treated with the most appropriate therapies, consider participation in clinical trials of new therapies, and to identify those most suitable for lung transplantation," the authors wrote.
They stressed, however, that the patients enrolled in their study were a highly selected cohort of patients suspected to have IPF and referred to regional sites for consideration of participation in a clinical trial. Therefore, the findings must not be extrapolated for all patients demonstrating the possible UIP pattern on HRCT images interpreted by general pulmonologists and radiologists in the community.



















