CHICAGO - Gallic genius, flair, and innovation came under the spotlight at the RSNA annual meeting on Monday during a celebration of France's many contributions to cancer imaging.
By her own admission, the French language skills of RSNA President Dr. Sarah Donaldson have become decidedly rusty since she spent a year of her fellowship at Institut Gustave Roussy (IGR) in Villejuif in the southern suburbs of Paris, but she valiantly threw herself into the session by speaking French. She said her time at IGR, spent learning about pediatric oncology, had the greatest personal and professional impact on her career as a physician-investigator, and was pivotal in shaping her life in academic radiation oncology.
 A hefty dose of Gallic charm enveloped McCormick Place on Monday, when four experts from France spoke at a special session about cancer imaging. Shown here are the two moderators, Dr. Jean-Pierre Pruvo (far right) and Dr. Nicolas Grenier (far left), and speakers Dr. Alain Luciani (second from left), Dr. Eric de Kerviler (third from left), Dr. Thierry de Baere (second from right), and Dr. Valerie Vilgrain.
A hefty dose of Gallic charm enveloped McCormick Place on Monday, when four experts from France spoke at a special session about cancer imaging. Shown here are the two moderators, Dr. Jean-Pierre Pruvo (far right) and Dr. Nicolas Grenier (far left), and speakers Dr. Alain Luciani (second from left), Dr. Eric de Kerviler (third from left), Dr. Thierry de Baere (second from right), and Dr. Valerie Vilgrain.Carrying on the central theme of Donaldson's opening address about the importance of patient care and collaborating with colleagues, Dr. Valerie Vilgrain discussed the role of the radiologist in the multidisciplinary team (MDT), particularly regarding colorectal liver metastases.
Significant growth in MDT working has resulted from increasing specialization, technological advances, and recommendations by national agencies, especially in the field of oncology, noted Vilgrain, who is head of radiology at the University Beaujon Hospital, Clichy. In France and elsewhere, radiologists have become key contributors to MDTs, and their presence is mandatory when discussing oncologic cases.
Based on extensive imaging workup and patient clinical status in cases of colorectal liver metastases, radiologists and hepatobiliary surgeons must discuss whether the patient is resectable, unresectable, or borderline. In unresectable or borderline patients, radiologists should evaluate tumor response to select the best treatment. In the future, morphologic and functional imaging may anticipate the histologic response.
"In colorectal liver metastases, the main goals are to assess resectability, to consider secondary resectability, and to evaluate tumor response," he said. "CT and MR imaging are essential, MR being the most sensitive for tumor detection. Further work has to be done to better analyze tumor response using functional imaging."
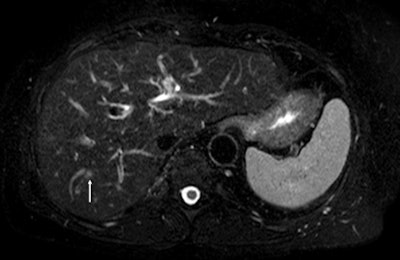 Fat-suppressed T2-weighted fast spin-echo MR image obtained in 61-year-old man with liver metastases from colorectal cancer. Only one metastasis in the right liver lobe is seen on this slice (arrow). Moreover, this lesion is barely seen because it is located next to a vessel. Images courtesy of Dr. Valerie Vilgrain.
Fat-suppressed T2-weighted fast spin-echo MR image obtained in 61-year-old man with liver metastases from colorectal cancer. Only one metastasis in the right liver lobe is seen on this slice (arrow). Moreover, this lesion is barely seen because it is located next to a vessel. Images courtesy of Dr. Valerie Vilgrain.
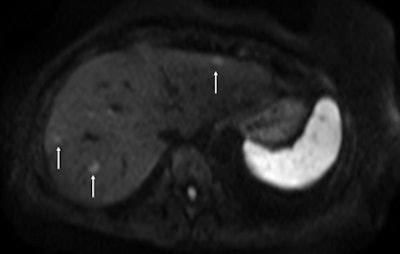 On the diffusion-weighted image, the same lesion is seen as well as two additional metastases: one in the right liver and one in the left liver. All metastases are strongly hyperintense compared to the background liver at b = 600 sec/mm2, indicating restricted diffusion. All of these lesions were surgically confirmed as metastases.
On the diffusion-weighted image, the same lesion is seen as well as two additional metastases: one in the right liver and one in the left liver. All metastases are strongly hyperintense compared to the background liver at b = 600 sec/mm2, indicating restricted diffusion. All of these lesions were surgically confirmed as metastases.Future trends in intra-arterial therapy of liver malignancies were outlined by Dr. Thierry de Baere, from the department of interventional radiology at the IGR. In the intra-arterial treatment of hepatocellular carcinoma, 3D angiography guidance with computer image analysis can improve outcomes of chemoembolization by better depicting liver tumors. Tumor feeding vessels can be depicted with a sensitivity of 93%, with the main limitation being in vessels smaller than 1 mm or when patients have been treated already, he explained.
Hepatic intra-arterial chemotherapy of colorectal liver metastases improves tumor response when compared with systemic chemotherapy; the treatment provides a response rate of 86% to 93% in these metastases, and more than half of patients can be operated on after intra-arterial chemotherapy, even though they were not surgical candidates before chemotherapy.
Such treatment can be proposed with minimally invasive placement of the catheter and port by the interventional radiologist, with functionality of ports equivalent to surgically placed ports. Traditionally, interventional radiologists have adapted drugs designed for intravenous use, but more research into drug and delivery platforms dedicated to intra-arterial delivery is needed, according to de Baere.
Clinical use of whole-body diffusion
In whole-body diffusion in hematology malignancies, both anatomic evaluation and routine functional tumor imaging are increasingly combined to provide definition of tumor staging and response, said Dr. Alain Luciani, professor of radiology at the University Paris-Est Créteil (UPEC).
Current MR techniques, including respiratory triggering, phased array coils, and parallel imaging, are bringing whole-body MRI into clinical practice, especially in oncology. Ongoing national and international protocols are being developed by French academic imaging groups, and whole-body diffusion-weighted MRI is being tested as a standalone sequence compared to PET/CT for aggressive lymphoma staging and follow-up in a bicentric French-Taiwanese research program, he pointed out.
Luciani described novel instrumental developments dealing with diffusion in hematologic malignancies. For instance, combining multiple b-factor acquisitions enables the extraction of both perfusion-related and true molecular diffusion parameters, following the intravoxel incoherent motion theory.
In hematologic malignancies associated with increased angiogenesis, such as multiple myeloma, both the perfusion fraction and the true molecular diffusion parameters can be used to monitor response to treatment. This approach is currently being investigated in a public-funded French study involving hematologic and radiologic teams, further highlighting the key role of whole-body MRI in the clinical management of patients with multiple myeloma, he said.
Biopsy guidance
Molecular imaging for biopsy guidance in oncology was the focus of the presentation by Dr. Eric de Kerviler, a radiologist at Saint-Louis Hospital in Paris.
Image-guided biopsies have become essential in the management of cancer patients, but the small amount of tissue taken in a heterogeneous tumor may be negative in a case of necrosis or fibrosis, or it may be positive but not represent the most aggressive component. The standard imaging modalities used for needle guidance are often adequate to identify the lesion or determine the needle trajectory, but they cannot overcome the variable expression of molecular targets within tumors.
Molecular imaging enables the visualization of the cellular function and the follow-up of the molecular process in living organisms, and it can offer a better insight into tumor biology, demonstrating areas of increased metabolism or cellularity, abnormal perfusion, and tissue stiffness. Combining morphological with functional imaging techniques for needle guidance can improve targeting and increase the diagnostic yield of biopsies, and it extends the field of indications of image-guided biopsies and offers new horizons to radiologists in the management of cancer patients, he said.
RSNA membership outside of North America has grown from 7% to 26% in the past 20 years, and more than 13,000 RSNA members now live outside of North America, according to Dr. Richard Baron, professor of radiology at the University of Chicago and RSNA's board liaison for international affairs, who concluded Monday's session.