Bone suppression computer-aided detection (CAD) software can provide a significant boost for diagnosis of pulmonary nodules, especially those of moderate and subtle conspicuity, Dutch researchers have reported.
In a study conducted at Radboud University Nijmegen Medical Center, posteroanterior (PA) and lateral digital chest radiographs of 111 patients (average age 65) with a CT-proven solitary nodule (median diameter 15 mm), and 189 controls (average age 63) were read by five radiologists and three trainees. The total number of missed lesions for the eight readers went down from 255 with chest x-rays (CXR) only to 189 with CXR and bone-suppressed images (BSI).
"The increase in sensitivity outweighed the non-significant loss of specificity," noted lead author Dr. Steven Schalekamp, from the department of radiology, in an article-in-press posted online on 25 September by the European Journal of Radiology. "All observers irrespective of their experience reached the best performance with BSI, also when evaluation was confined to a high specificity range."
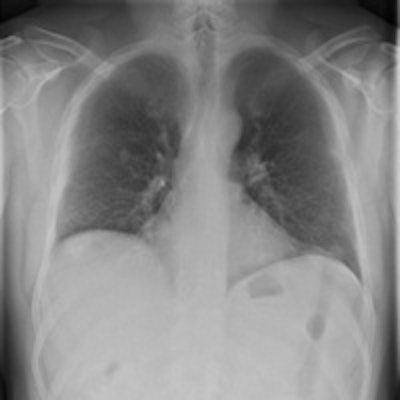
 A 12-mm nodule in the right lung is completely obscured by overlying bone structures. The bone suppression software suppressed the ribs and improved the visibility of the nodule. All images courtesy of Dr. Steven Schalekamp.
A 12-mm nodule in the right lung is completely obscured by overlying bone structures. The bone suppression software suppressed the ribs and improved the visibility of the nodule. All images courtesy of Dr. Steven Schalekamp.In general, a chest x-ray is not taken to detect nodules, but they should be reported because solitary lung nodules, in the size range detectable by CXR, harbor a high risk to represent early stage lung cancer. A substantial number of bronchogenic tumors are missed on the initial radiograph, even though they are visible in retrospect, and the actual frequency of lung cancers missed on CXR ranges from 19% to 26%, according to Schalekamp and his colleagues.
"Obscuration of lung cancer by overlying bone structures represents a major contributor to misdiagnosis," they pointed out. "A new software product has been developed to suppress ribs and clavicles in the original image without requiring special hardware or increase of patient dose caused by double exposures."
All chest radiographs were obtained with a digital technique using storage phosphor computed radiography plates (Agfa Healthcare), Selenium drum (Thoravision, Philips Healthcare) and flat panel detector digital radiography systems (Siemens Healthcare). Radiographs were obtained using 120 or 125 kVp, respectively, with automatic exposure control.
Bone suppressed images were generated by ClearRead Bone Suppression 2.4 (Riverain Technologies). This software uses advanced image processing to construct a bone suppressed PA chest image, and it can produce an image that has the same characteristics as the original image with respect to gradation, detail contrast, and size. It has U.S. Food and Drug Administration (FDA) approval.
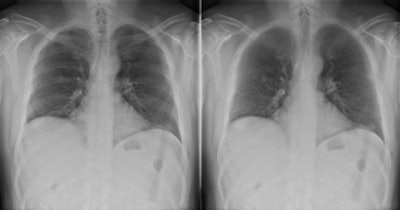
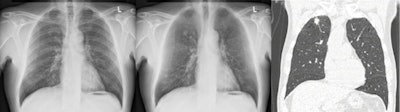 Example case in which the radiologists improved their detection of a 13 mm, pathologically proven, squamous cell carcinoma in the right upper lobe.
Example case in which the radiologists improved their detection of a 13 mm, pathologically proven, squamous cell carcinoma in the right upper lobe.The five radiologists had between three and 17 years' experience, and they were accompanied by one second-year and two third-year trainees. The readers evaluated 300 study cases in different randomized orders. Before the reading sessions, they evaluated a training set of 40 cases with and without BSI. During this training session, the researcher gave instantaneous feedback to the observers. None of the observers had previous experience in reading CXR with BSI, or dual energy chest radiography. Readings were carried out using a 30-inch (Flexscan SW3031W, Eizo) DICOM-calibrated LCD monitor in a darkened room, the authors wrote.
They classified the conspicuity of nodules as obvious (n = 32), moderate (n = 32), subtle (n = 29), and very subtle (n = 18). Observers read the PA and lateral chest radiographs with and without an additional PA BSI within one reading session.
Receiver operating characteristic (ROC) analysis showed improved detection with use of BSI compared with CXR alone (AUC = 0.883 versus 0.855; p = 0.004). Performance also increased at high specificities exceeding 80% (pAUC = 0.136 versus 0.124; p = 0.0007). Operating at a specificity of 90%, sensitivity increased with BSI from 66% to 71% (p = 0.0004). Increase of detection performance was highest for nodules with moderate and subtle conspicuity (p = 0.02; p = 0.03).
Average nodule diameter was 16 mm (7.8 mm to 34.9 mm), with a median of 15 mm. Five nodules exceeded a diameter of 30 mm and could be classified as a mass, Schalekamp et al stated. A total of 80% of the nodules were malignant, which was histologically proven in 85% of cases and based on clinical history in 15% of cases. There were 25 apical nodules located in the cranial of the aortic arch, 15 (peri) hilar nodules, nine retrocardiac nodules, and 62 peripheral nodules located in the remaining lung fields. Of all lesions, 31% (n = 35) were minimally and 69% were partially to completely (n = 76) superprojected by bones. The degree of superprojection by bones was not statistically correlated with conspicuity.
The study suffers from limitations, the authors conceded. First, they studied a selected patient group. Although all cases were derived from clinical workup, the prevalence of nodules was substantially higher than in clinical practice. Also, only one nodule per case was present, and this might have affected observers' behavior. Furthermore, it is less likely that observers missed nodules due to inattention, which may be an important factor in clinical practice. Finally, observers had no experience with BSI. Although a training set of 40 cases was provided, more training might be needed to learn about the strengths and weaknesses of BSI.
"We are doing multiple studies trying to improve detection of abnormalities in chest radiographs," Schalekamp noted in an email to AuntMinnieEurope.com. "We are working on a paper about computer-aided detection for the detection of lung nodules. We are also testing the effect of BSI on the detection of other abnormalities. Further, we are exploring the potential use of these two techniques, bone suppression software and computer-aided detection, in clinical practice."
Study disclosure
Riverain Technologies provided a research grant to Nico Karssemeijer from Nijmegen, one of the co-authors of this study. The first author was hired from this research grant. The company had no influence on the execution of the study or the decision to submit this paper for publication. Data and analysis were managed by the authors.