The largest study to probe the effects of ionizing radiation since the atomic bomb survivor studies shows that cancer incidence does rise among younger patients -- although only in small amounts -- in the years following their exposure to CT scans, according to an Australian article published yesterday in BMJ.
Researchers studied the records of nearly 700,000 children and young adults who had CT examinations between 1985 and 2005, finding more than 60,000 cancers including 3,150 that occurred at least one year after a CT scan. They compared these records with those of more than 10 million people who were not scanned. After accounting for a wide range of demographic factors, they found the overall cancer incidence in this group was 24% higher than for unexposed individuals, with the greatest increases seen in brain cancer and several solid organ cancers, as well as in younger patients.
"Our study shows that CT scans during childhood and adolescence are followed by an increase in cancer incidence for all cancers combined and for many individual types of cancer," wrote Dr. John Mathews, professorial fellow and epidemiologist at Melbourne Medical School, and colleagues from several other Australian institutions. "We cannot, however, necessarily assume that all the excess cancers seen during the current period of follow-up were caused by CT scans, because scanning decisions are based on medical indications and are not allocated at random," (BMJ, 21 May 2013).
Still, the finding that cancer incidence was linked to the site of the irradiation showed that the scans themselves were likely to be the cause of many of the post-CT malignancies recorded during the mean 9.5-year follow-up, the group wrote, cautioning that the precise cost of the scans cannot be determined as the malignancies continue to appear over time.
An accompanying editorial by Dr. Aaron Sodickson, section chief of emergency radiology and medical director of CT at Brigham and Women's Hospital in Boston, lauded the study's careful assessment of cancer data as an excellent step toward clarifying the effects of CT radiation, but said that capturing real-time information on radiation exposure over time would provide even better data going forward.
"Such data capture would also enable more accurate patient-specific dose estimation than was possible from the data sources available to Mathews and colleagues," Sodickson wrote. "Although the authors assigned credible doses to the scans in their study, future epidemiological work may be greatly enhanced by improved capture of patient-specific dosimetry" (BMJ, 21 May 2013).
"With further validation of radiation risk models, not only in children but also in adults, we will ultimately be able to perform more accurate patient-specific risk assessment to better inform imaging decisions," Sodickson continued. "Mathews and colleagues' study is a vital step towards this goal."
Data still unclear
Some recent studies have offered estimates of the risks associated with low doses of ionizing radiation, including a U.K. study of 180,000 showing increasing incidence of leukemia and brain cancer that mirrored medical doses received. But some have questioned the validity of this and other studies, and much uncertainty remains.
Mathews and colleagues looked at Australian Medicare records over 20 years in an effort to provide clearer long-term answers about the effects of CT radiation, specifically assessing cancer incidence among individuals exposed to CT more than a year before a cancer diagnosis compared with the unexposed population. To arrive at estimated effective exposures, scanner settings were estimated based on common practice including reduced exposure settings for younger patients.
The 10.9 million people identified from Australian Medicare records were all between the ages of 0 and 19 years in January 1985, or born between then and December 2005. From this group, the authors identified 680,211 individuals exposed to CT scans, linking the data through national medical records to 3,150 scanned patients who were diagnosed with cancer at least a year after CT through the end of 2007, with a mean follow-up of 9.5 years.
Cancer incidence higher for scanned patients
The overall cancer incidence was 24% greater for exposed individuals compared with unexposed people, after accounting for age, sex, and year of birth, for an incidence rate ratio (IRR) of 1.24 (95% confidence interval 1.20 to 1.29; p < 0.001). Moreover, the IRR increased by 16% (0.13 to 0.19) with each additional CT scan (p < 0.001 for trend), the study team reported. The increased incidence did not disappear over time for the exposed patients, although it slowed.
"When the calculations were repeated based on lag periods of five and 10 years, cancer incidence remained higher in the exposed group than in the unexposed group, although the proportional increases were smaller compared with those based on the one-year lag period," they wrote. Thus, for the five-year lag period the IRR was 1.21 (1.16 to 1.26, p < 0.001) versus 1.18 (1.11 to 1.24, p < 0.001) for the 10-year lag period.
The IRR for exposed individuals versus the unexposed rose not only for all cancers combined but for solid cancers, lymphoid, and blood-based cancers looked at separately.
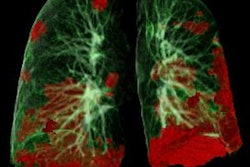
Brain cancer showed the highest increase in IRR, with other significant increases in cancers of the digestive organs, melanoma, soft tissue, female genital organs, urinary tract, thyroid, and ill-defined or unspecified sites, as well as Hodgkin's lymphoma, other lymphoid cancers, leukemias, and myelodysplasias.
Brain cancer shows sharpest increase
Almost three-fifths of the scans were of the brain, so the authors performed a new analysis excluding these. The IRR for brain cancers after the patient was scanned in another anatomic site remained elevated (IRR 1.51) as did IRRs for all solid cancers (IRR 1.19) and all cancers (IRR 1.20).
On the other hand, the authors found a highly significant reduction in IRR for all solid cancers except brain cancer after a CT scan as the age of exposure increased (p = 0.01 for trend). However, there was no significant trend in the absolute excess incidence rate (EIR) with increasing age at exposure. For brain cancer as well as for all cancers combined, IRRs were highest for CT exposures in children younger than 5 years, and the risk fell with increasing age at the first CT exposure (p = 0.001 for brain cancer, p < 0.001 for trend for all cancers). In fact for all cancers, IRR decreased with increasing age, though it remained higher than unexposed individuals for all cancers.
"Our study shows that CT scans during childhood and adolescence are followed by an increase in cancer incidence for all cancers combined and for many individual types of cancer," Mathews and colleagues wrote. "We cannot, however, necessarily assume that all the excess cancers seen during the current period of follow-up were caused by CT scans, because scanning decisions are based on medical indications and are not allocated at random."
As a result, reverse causation -- whereby symptoms of precancerous conditions are evaluated by CT -- cannot be ruled out, and this effect is most likely for brain cancers, where symptoms prompting a CT scan might appear years before cancer manifests.
Controls don't account for differences
Several study observations do make it likely that CT scans cause most of the excess cancers. These include the finding that IRR increased with an increasing number of scans -- the finding that younger patients were hit with larger proportional increases in cancer incidence as seen in the Japanese bomb survivor data. In addition, the study showed a larger absolute EIR in female patients versus male patients exposed to CT, and that the site of the CT scans was correlated to the cancer site, with a large increase in EIR for leukemias and myelodysplasias following exposure of the red bone marrow after CT scans of the abdomen and pelvis.
"This observed increase in risk associated with the low radiation doses delivered by CT scans supports the most widely adopted linear-no-threshold dose-response model in which double the radiation dose is assumed to impart double the cancer risk," Sodickson wrote in his editorial. "The reported risks also roughly match the lifetime attributable risks predicted by the BEIR-VII (biological effects of ionizing radiation) report; one of the most commonly used linear-no-threshold models."
The finding that will generate the most headlines is that childhood exposure boosts the incidence of cancer by 24%, he continued. "However, it is important to recognize that the baseline incidence of cancer in a general pediatric population is extremely small, so that a 24% increase makes this risk just slightly less small."
Clear message for physicians
Doctors will increasingly need to weigh the benefits of CT against the potential risks, Mathews and colleagues noted.
"Fortunately, many radiologists are now aware of the risks, and technological advances have already allowed CT scan doses to be reduced below those used in earlier decades," they wrote. "However, decision tools to objectively assess the need for CT are still not used routinely."
Sodickson stated there are many opportunities before, during, and after scans to cut exposure, and that physicians must make use of every opportunity to do so. Dosimetry, the collection of cumulative exposure data, and rigorous adherence to evidence-based scanning decisions represent important opportunities.
"Imaging algorithms or evidence-based clinical decision rules may be adopted for clearly defined clinical scenarios. Electronic decision support embedded in the scan ordering process can substantially reduce utilization," he wrote.