Patients with extracardiac arterial disease (ECAD) have a high prevalence of occult coronary artery disease and may benefit from early detection, Dutch researchers said at last month's ECR 2013.
While these patients aren't routinely screened for coronary artery disease, screening might prevent a significant amount of morbidity and mortality, said researchers from University Medical Center Groningen in the Netherlands. More than half of the patients in their study had either a high calcium score or significant coronary artery stenosis, they concluded.
"Extracardiac arterial disease is very common finding, especially in aging patients, and studies have shown that patients with ECAD have a high risk of coronary artery disease," said doctoral candidate Dr. Martijn den Dekker in his ECR presentation. In fact, coronary artery disease is a major cause of death in these patients, he added.
"So possibly detection of CAD [coronary artery disease] in preclinical asymptomatic phase could reduce cardiac morbidity and mortality in vascular patients," especially since modalities such as CT and MRI make noninvasive screening possible on a large scale, den Dekker said.
The prospective study aimed to assess the prevalence of silent significant CAD in patients with ECAD using coronary CT angiography (CCTA) and adenosine stress MRI.



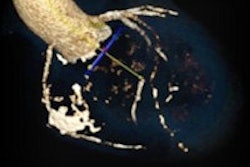
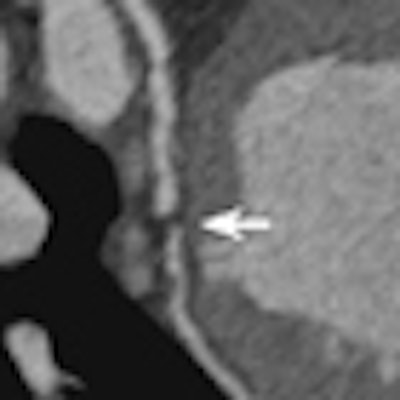
 A 64-year-old patient with carotid stenosis. Top left: Coronary CT angiography image. White arrow points to a soft plaque in the midcircumflex artery, with stenosis of the lumen. Calcium score was 64. Top right: Short-axis image of the adenosine perfusion MRI examination. White arrow points to a perfusion defect in the posterolateral wall, during stress. The perfusion defect was not present in the rest series, thus indicating inducible ischemia. Bottom left: Invasive coronary angiography image of the left coronary arteries. Black arrow points to a significant stenosis, corresponding with the location seen on CT. Bottom right: Invasive coronary angiography image after intervention. Good results were achieved after percutaneous coronary intervention with stent placement. All images courtesy of Drs. Rozemarijn Vliegenthart and Martijn den Dekker.
A 64-year-old patient with carotid stenosis. Top left: Coronary CT angiography image. White arrow points to a soft plaque in the midcircumflex artery, with stenosis of the lumen. Calcium score was 64. Top right: Short-axis image of the adenosine perfusion MRI examination. White arrow points to a perfusion defect in the posterolateral wall, during stress. The perfusion defect was not present in the rest series, thus indicating inducible ischemia. Bottom left: Invasive coronary angiography image of the left coronary arteries. Black arrow points to a significant stenosis, corresponding with the location seen on CT. Bottom right: Invasive coronary angiography image after intervention. Good results were achieved after percutaneous coronary intervention with stent placement. All images courtesy of Drs. Rozemarijn Vliegenthart and Martijn den Dekker.Two centers in the Netherlands scanned 115 cardiac-asymptomatic patients age 50 years and older (mean age 65 years; 76% men) with proven aneurismal or stenotic arterial disease with CT, MRI, and sometimes echocardiography as well.
The patients completed a questionnaire, and data were collected on their height, weight, blood pressure, C-reactive protein, and ECG results. Patients were excluded from the study if they had a history of acute coronary syndrome, cardiac complaints, severe hyper- or hypotension, or contraindications for CT or MRI.
All patients underwent calcium scoring. Those scoring less than 1,000 proceeded to CCTA, while those with scores greater than 1,000 were referred for adenosine perfusion MRI.
Patients undergoing CCTA also underwent adenosine perfusion MRI, unless significant left main stenosis or equivalent was found, den Dekker said. If so, they were referred to the cardiologist without stress testing. Perfusion defects seen at MRI also earned patients a visit to the cardiologist, he said.
Patients were divided into two categories: stenotic (n = 87) and aneurismal ECAD (n = 28). The stenotic group was subdivided into those with peripheral arterial occlusive disease (PAOD) (n = 71) or carotid stenosis (n = 16).
A total of 86 patients underwent MRI, and 21 patients were referred to the cardiologist, one with significant left main artery stenosis, 10 with other ischemic coronary stenosis at MRI, and 10 for other indications. CCTA was positive in 38% of the stenotic patients and 29% of the aneurismal ECAD patients. Heavy calcium precluded CCTA in 20% of patients.
Of the 150 patients who completed calcium scoring, 23 (39.4%) had scores higher than 1,000, and 29 patients underwent CCTA.
Two patients, including one stenotic and one aneurismal ECAD patient, had left main stenosis. Adenosine perfusion MR was positive in 12% of stenotic and 11% of aneurismal ECAD patients, while 18% of stenotic and 21% of aneurismal ECAD patients were referred to the cardiologist.
Cardiac interventional procedures were performed in 43% of stenotic and 33% of the aneurismal ECAD patients, and either a significant stenosis or high calcium score was found in 58% of stenotic versus 50% of aneurismal ECAD; however, none of these outcomes was statistically significant, den Dekker said.
In all, 42% of the PAOD cases were referred for intervention, versus half of the carotid stenosis cases and 21% of the aneurysm, the group reported.
Imaging results
|
"There is a high prevalence of silent severe coronary artery disease in patients with ECAD, and furthermore this prevalence is not significantly different for stenotic versus aneurismal ECAD," den Dekker said.
Screening in these high-risk patient groups, may be beneficial; however, further studies are needed first, he concluded.
In response to a question from the moderator about the clinical significance of the findings, and how they might be applied, den Dekker said these patients need to be identified early because most PAOD have a limited range for walking that can obscure a diagnosis of heart disease until very late in the game.
"Cardiac complaints with these patients reveal themselves at a later stage, so when they become symptomatic, it is already too late, and they present with cardiac infarction," he said.
An audience member commented there aren't many good avenues for introducing screening for vascular disease, because searching for coronary artery disease in patients with an abdominal aortic aneurysm will produce an obstructive disease rate of more than 50%, and if you put a stent in a patient who might need surgery a year later, you're introducing more risk and variables.
Good, creative, prospective studies are needed to try to find ways to trim the event rate in this group of patients, the commenter said.