A study from the Netherlands has shown that evaluating vascular cross-sectional area differences of internal mammary vessels could be a new predictor for malignancy on MRI. The measurement was significantly different in breast cancer patients on the side with cancer compared with the contralateral side, and the variation was not evident in healthy controls.
Breast MRI is an important part of the diagnostic workup in breast cancer patients. One way to use MRI is to measure breast vascularity, as it is often associated with breast cancer. Researchers usually use two methods to assess changes in vascularity: prominent vessels leading to an enhanced lesion, and imaging the vascularity of the whole breast on both sides with contrast-enhanced MRI. However, both techniques have shortcomings according to the researchers (Insights into Imaging, 16 January 2013).
In healthy women, the breast is mainly perfused by the internal mammary artery (IMA), according to Dr. Robert-Jan Schipper from the department of surgery at Maastricht University Medical Center, the Netherlands, and colleagues. It's a paired artery, one running on the left side of the sternum and one on the right side.
"We hypothesized that if a malignant lesion is present the cross-sectional area of the IMA and/or internal mammary veins (IMV) on the side of the lesion is increased compared to the healthy side," they wrote. "Measuring and comparing the left and right IMA and IMV could only be useful if the cross-sectional areas of these vessels in a healthy person without breast malignancy are similar."
The cross-sectional areas of the IMA and IMV were measured on the left and right side in the second and third intercostal space (ICS) of 135 breast MRIs by two independent readers.
In the healthy control group (n = 91) no significant differences were observed between the cross-sectional areas of the IMA and IMV. Both readers reported a mean adjusted difference of 0.12 mm2 and 0.21 mm2 for the IMA in the second intercostal space.
In the malignancy group (n = 44), the cross-sectional area was significantly larger on the malignancy side compared with the contralateral side. The largest difference in the IMA was measured in the second intercostal space with a mean adjusted difference for reader one of 1.37 mm2 and 0.81 mm2 for reader two.
"With this knowledge bilateral comparison of the internal mammary vessels evaluated in the second and third ICS might be used as a predictor for the presence or absence of malignancy," the researchers wrote. "Based on these results it seems most appropriate to focus on the IMA."
The IMA showed the biggest enlargement of the cross-sectional area compared with the IMV. As far as location, the enlargement of the IMA is more explicit in the second intercostal space compared with the third, they noted. Plus, the method is not time-consuming; only two measurements of the IMA are needed, the left and ride side, which take about a minute.
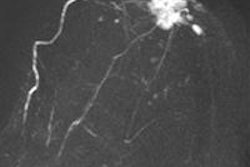
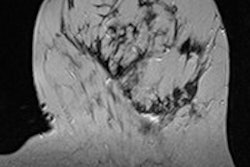
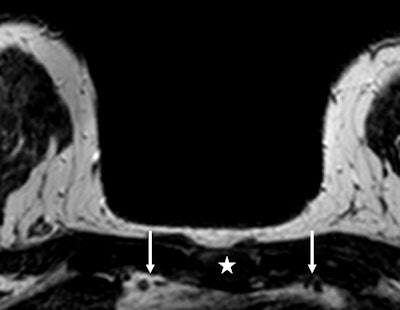 An example of the measurement of the cross-sectional area of the internal mammary vessels in a patient with a right-sided breast lesion of 1.9 cm. With sagittal reconstruction, the manubrium was marked (white star), which appears automatically in the transverse slices. On the transverse slice, using the marker the second intercostal space is recognized and the cross-sectional area of the internal mammary vessels (left and right arrows) can be measured. In this patient, the right internal mammary artery measured 5.21 mm2, compared with the left internal mammary artery of 4.12 mm2. Histopathology showed an invasive ductal carcinoma. Image courtesy of Dr. Robert-Jan Schipper.
An example of the measurement of the cross-sectional area of the internal mammary vessels in a patient with a right-sided breast lesion of 1.9 cm. With sagittal reconstruction, the manubrium was marked (white star), which appears automatically in the transverse slices. On the transverse slice, using the marker the second intercostal space is recognized and the cross-sectional area of the internal mammary vessels (left and right arrows) can be measured. In this patient, the right internal mammary artery measured 5.21 mm2, compared with the left internal mammary artery of 4.12 mm2. Histopathology showed an invasive ductal carcinoma. Image courtesy of Dr. Robert-Jan Schipper.However, measurement of the internal mammary vessels has its shortcomings. "First of all, it is not possible in patients who have undergone a coronary artery bypass graft," Schipper and colleagues wrote. "After unilateral mastectomy, it is also not possible to make a reliable left-right comparison of the internal mammary vessels. It is unclear whether tissue sampling in the breast influences the cross-sectional area of the internal mammary vessels because of an inflammation reaction after sampling."
Another shortcoming is that only the internal mammary vessels were investigated, although the breast is supplied by both the IMA and the lateral thoracic artery (LTA). Scientific literature suggests measurement of the IMA is not sufficient in some patients, and measurements of the left thoracic artery are needed.
"However, it would be very difficult to measure the LTA," Schipper and colleagues wrote. "Because of the anatomy of the LTA, a standardized location for measurements is not available so inter- and intraobserver variability will not be as good compared to the measurements of the IMA."
Plus, visualizing a tumor within the breast could introduce bias in the measurement -- for instance, overestimation of the cross-sectional areas at the side of the breast cancer.
"Ideally, measurements of the vessels should be performed without visualization of the breast itself," the researchers continued. "However, this is not possible within our viewing workstations."
A future study should prospectively confirm their retrospective results in a larger cohort, the researcher said. "In addition, we would suggest evaluating the possible correlation between tumor diameter and cross-sectional vessel enlargement or assessing the differences between various types of breast cancer, i.e., invasive versus in situ cancers," they noted.
Schipper and colleagues concluded that their technique may improve the specificity of breast MRI. However, "we wish to emphasize that this is only speculative and that this theory should be evaluated in a larger prospective study, especially with the addition of this new parameter to the common used BI-RADS lexicon parameters."