New research from the U.K. has revealed radiographer-led immediate (or "hot") reporting in the emergency room can cut overall hospital costs, reduce treatment errors, and improve doctor confidence. Furthermore, if radiographer reporting roles were expanded to chest and abdomen radiographs, where a greater number of interpretive errors are known to occur, the total savings could be substantial.
 Figure 1A: False-negative outcome after a knee radiograph. The patient within the standard delayed reporting arm was discharged by the accident and emergency (A&E) clinician as normal for further A&E review if required. All images courtesy of Maryann Hardy, PhD.
Figure 1A: False-negative outcome after a knee radiograph. The patient within the standard delayed reporting arm was discharged by the accident and emergency (A&E) clinician as normal for further A&E review if required. All images courtesy of Maryann Hardy, PhD.
"Whichever way you look at it, improving radiography practices has a knock-on effect, not just in reducing costs but also improving quality throughout the hospital," said Maryann Hardy, PhD, professor of radiography and imaging practice research and director of postgraduate research at the School of Health Studies, University of Bradford. "This is not just about releasing radiologists, but also about using radiographers' skills differently and effectively to benefit the service -- and this is the first study which has [assessed] immediate radiographer-led reporting and its impact on outside departments."
In the U.K., radiographers are already responsible for some accident and emergency (A&E) reporting, with 63% of hospitals already employing reporting radiographers. While this phenomenon has advanced radiographer practice, the mirroring of delayed reporting common among radiologists did little to improve the service or inform patient management, wrote Hardy and colleagues in the current issue of Radiography (February 2013, Vol. 19:1, pp. 23-27).
"Delayed reporting increases the risk of clinical errors, namely missed diagnoses and in unclear cases, overtreatment. We wanted to see if using radiographer skills differently and implementing an immediate reporting service could reduce these errors, improve confidence in patient management, and make savings that would impact the entire hospital, not just the radiology department," she explained.
 Figure 1B: Tibial plateau fracture with visible lipohemarthrosis was identified on image review. The patient was recalled to A&E for orthopedic intervention several days later.
Figure 1B: Tibial plateau fracture with visible lipohemarthrosis was identified on image review. The patient was recalled to A&E for orthopedic intervention several days later.Part of a randomized controlled trial, the study, which began in 2009, focused on musculoskeletal (MSK) patients who underwent radiographic imaging and were then divided into two reporting arms, standardized (delayed) and immediate. A total of 1,502 patients from five hospitals within three National Health Service (NHS) Trusts (or groups of hospitals) across the north of England were included in the final study analyses. Of these, 752 patients, accounting for 839 examinations, were recruited to the immediate reporting arm and 750 patients (849 examinations) were recruited to the delayed reporting arm, with follow-up conducted by means of a questionnaire at eight weeks postattendance date for the evaluation of short-term injury recovery status.
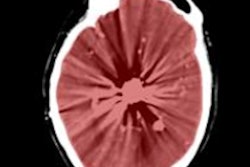
 False-positive outcome after a hand radiograph. The patient within the standard delayed reporting arm was identified as having a fracture to base of second metacarpal and referred for hand surgery opinion and intervention. Appearances reported as normal pseudoepiphysis. The patient was later discharged.
False-positive outcome after a hand radiograph. The patient within the standard delayed reporting arm was identified as having a fracture to base of second metacarpal and referred for hand surgery opinion and intervention. Appearances reported as normal pseudoepiphysis. The patient was later discharged.
The study showed that patients in the immediate reporting arm benefited from more accurate diagnoses, with no recalls to the A&E, and more appropriate management by doctors, which reduced costs particularly through a reduction in short-term bed stays.
"The cost savings in the immediate reporting arm worked out at 23.70 pounds (28.3 euros) per patient, which sounds small but considering that approximately 20 million patients attend A&E in England and 50% of these will be referred for imaging, 5 million of whom are likely to be MSK patients, then this saving would work out at overall hospital savings of 117 million pounds (139.6 million euros) across NHS organizations," she pointed out.
If radiographer reporting roles were expanded to include chest and abdomen radiographs where a greater number of interpretive errors are known to occur, and if the system was rolled out to all A&E patients, the overall savings would be substantial, according to Hardy.
The study also aimed to establish if the cost-savings and benefits would outweigh the investment needed to establish a new radiographer-led MSK image reporting service in hospitals that did not already use such a reporting model. It found that employing six high-grade radiographers to provide an immediate reporting service for 20,000 MSK examinations per year would still generate an average 200,000 pounds (238,600 euros) per year saving to a hospital trust.
 Maryann Hardy, PhD, argues the case for expanding the remit of radiographers to include immediate chest and abdomen radiograph interpretation for A&E patients.
Maryann Hardy, PhD, argues the case for expanding the remit of radiographers to include immediate chest and abdomen radiograph interpretation for A&E patients.
A subsequent survey of A&E doctors pointed to high satisfaction with radiographer-led immediate reporting: The greater presence of the radiographer in the clinical setting allowed clinicians a higher degree of ease and confidence in approaching the reporting radiographer with any questions, while radiologists were seen as less accessible in case of queries, according to Hardy.
Interest in radiographer reporting and the outcomes of the recent study is gaining increasing international interest, particularly from countries where radiologists are in limited supply.
Looking ahead, there was no reason for radiographers not to become involved in reporting for other types of patients besides MSK, according to Hardy. Mid Yorkshire Hospitals Trust, which was involved in the randomized trial, has continued with radiographer-led hot reporting, not just in emergency MSK patients, but also in chest and abdomen, where greater and more serious errors and poorer patient outcomes may occur with delays between imaging and reading.
"We anticipate that even greater savings could be made through a radiographer-led reporting service for chest and abdomen images and in future hope to have a cohort ready for research and evaluation," she said.