Imaging in battle zones is developing fast, both in terms of quality and quantity. More military conflicts call for more onsite radiology, and with that the need for better quality care. Multidetector-row CT (MDCT) and focused abdominal sonography in trauma (FAST) allow physicians to better triage and treat patients, according to a new article.
Imaging in countries such as Iraq or Afghanistan carries its own special challenges, including supply shortages, power outages, and -- depending on the intensity of skirmishes -- multiple patients requiring immediate attention at once. Dr. Richard Graham, a consultant radiologist from the Royal Naval Reserve and the radiology department at the Royal United Hospital in Bath, U.K., shared his experiences in Afghanistan during the summer of 2010 in a pictorial review published online by the British Journal of Radiology on 17 July 2012.
Dr. Graham found plain film and ultrasound are useful modalities for imaging battlefield injuries, but MDCT has significantly increased the clinical input that radiologists can offer in battlefield trauma.
 These two images are from a soldier in a vehicle hit by an improvized explosive device. Above: A lateral CT reformat of the cervical spine with an anterior inferior fracture of C5. Below: A coronal CT reformat of the sacrum and lumbar spine. The patient demonstrates a left vertical sacral fracture, left transverse fracture of L5, and burst fracture of L2. All images courtesy of Dr. Richard Graham.
These two images are from a soldier in a vehicle hit by an improvized explosive device. Above: A lateral CT reformat of the cervical spine with an anterior inferior fracture of C5. Below: A coronal CT reformat of the sacrum and lumbar spine. The patient demonstrates a left vertical sacral fracture, left transverse fracture of L5, and burst fracture of L2. All images courtesy of Dr. Richard Graham.
"It is extremely difficult to manage battlefield trauma well without MDCT, as many nonclinically obvious injuries will go undiagnosed or patients will suffer from unnecessary exploratory surgery," he wrote. "Interventional vascular radiology is being used in Afghanistan. It is not known whether it produces enough benefit to justify the resources required to provide it as a deployed service."
In the past, MDCT images from the U.K.-run military hospitals in Iraq and Afghanistan were reported remotely because the conflict intensity was low and staffing of military radiology was limited, according to Graham. Using this remote reporting system, authorized results were with the referring clinicians within one hour, at any time of the day, seven days a week. As is often the case, FAST was performed by nonradiologists, usually general surgeons or radiographers who had undergone training.
In 2009, the decision to deploy radiologists to Afghanistan was made because the one-hour turnaround was not rapid enough, and it became difficult to coordinate the imaging of multiple casualties simultaneously.
The U.K. military hospital at Camp Bastion treats the armed forces of the NATO International Security Assistance Force, locally employed civilian contractors, captured enemy combatants, and some local nationals, Graham wrote.
"Battlefield radiology is like any other field of radiology in that it requires specific knowledge of etiology (mechanism of injury), common patterns of disease (injury patterns), and what not to miss," he noted.
The radiology department at the Camp Bastion military hospital comprises two consultant radiologists and about six radiographers. Normally, three radiographers are on shift during the day and evening. Overnight, one radiographer is in the department, with others on call if help is needed, he said. All the radiographers can do MDCT and plain film. The radiologists alternate between 24 hours first on and 24 hours second on.
"The radiographers receive training in CT before deployment to ensure familiarity with the particular scanners they will be using," he wrote. "Both radiologists and radiographers undergo about one month of predeployment military skills training."
Graham goes into detail about the many types of modalities in use at Camp Bastion, but in essence the camp is equipped with the following:
Direct digital radiography portable machines whose images can be viewed initially on nondiagnostic, built-in screens before uploaded to PACS for reporting.
Ultrasound systems using curvilinear abdominal and linear high-frequency probes, with the consultant radiologist performing nearly all the diagnostic ultrasound scans. If other staff members are trained, they perform the scan and ask the radiologists' opinion if required.
Digital subtraction angiography is undertaken if arterial injury is discovered intraoperatively or the surgeon would like to image a repaired vessel. An on-table angiogram can be formed using an image intensifier.
Two MDCT scanners (LightSpeed 64-slice, GE Healthcare), which permits increased scanning throughput at times when multiple casualties arrive at once. However, only stable patients are scanned. The most severely injured patients (about two-thirds) receive a traumagram.
"In practice, most imaging occurs between 20 and 60 minutes after patient arrival at the hospital door," Graham noted. The consultant radiologist does an initial read to identify potentially life-threatening findings and then the surgical team is notified, which takes about one to two minutes. The report is verbal, and the spine is not cleared yet. A detailed read is then undertaken, and a report is typed on the RIS and issued, which takes between 20 and 60 minutes depending on the degree of injuries.
"MDCT is used to exclude immediately life-threatening and less critical injuries that will require treatment later," he said.
Reporting the positions of the endotracheal tube, nasal airways, oral airways, venous catheters, arterial catheters, intrasosseous needles, pleural drains, and urinary catheters is important, as misplaced lines and tubes can cause serious harm to the patient, he noted.
Types of injury
The injuries most frequently seen at Camp Bastion are from blasts, gunshot wounds, and blunt trauma. There is also a group of patients who have contracted disease while on operations and not as a result of battlefield injury, known as disease nonbattlefield injury patients.
Blast injuries are generally caused by improvised explosive devices (IEDs), which are "homemade" bombs, intended to severely injure or kill. Blast injuries can be classified as primary, secondary, tertiary, and quaternary. Primary blast injury is from the abrupt increase in air pressure due to the explosion. Damage occurs to the organs that have gas/soft-tissue interfaces, such as the lungs and gastrointestinal tract, Graham noted.
Secondary blast injury results from fragmentation of the IED or from adjacent debris gaining kinetic energy and causing injury by penetrating trauma.
Tertiary blast injury occurs when the patient is thrown as a result of the blast injury or collides with objects in the immediate vicinity. Tertiary blast effects most commonly afflict soldiers in vehicles.
Quaternary blast injury results from thermal effects, toxic effects, or any postincident risks, such as drowning or freezing.
"IEDs produce catastrophic injuries to troops who are on foot (dismounted troops)," Graham wrote. "If the soldier is directly over the blast as it occurs, both lower limbs tend to be traumatically amputated (normally below the knee), as is the right arm and several fingers from the left hand. This pattern of injury in the upper limbs occurs because the right hand is holding the pistol grip of the rifle close to the soldier's body and left hand is further forward holding the rifle, and thus is just outside the center of the blast wave."
Other injuries that can occur during a blast are to the head and neck, spine, chest, abdomen, and pelvis.
In terms of gunshot wounds, helmets and body armor protect the anterior, posterior, and lateral chest, as well as the head from the forehead to the occiput. Therefore, injuries tend to occur in the face, axilla and abdomen/pelvis, buttocks, and limbs. Local nationals without body armor can have gunshot wounds anywhere.
As with blast injury, systematic evaluation of the CT scan is advised.
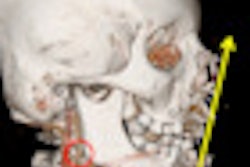
"Patients with facial injuries who reach the emergency department alive usually have not had their cranial fossae breached, and their injuries normally involve just the facial skeleton," Graham said. "Basal skull and skull vault fractures are commonly associated, but tend to be simple fractures rather than depressed fractures or large holes in the skull."
Facial fractures tend to be complex, involving the maxilla, mandible, and zygoma. The eyes should be carefully evaluated for ocular trauma. Oral fragments are common and should be reported, as they signal a risk of aspiration.
Battlefield blunt trauma is similar to civilian blunt trauma -- road traffic collisions and falls from height are similar to those seen in civilian practice.
Nonbattlefield injuries also occur, and because the majority of soldiers are males 18 to 40 years old, the diseases that manifest themselves in an operational environment that require imaging are relatively few. The most common are renal tract stone disease, appendicitis, and epididymo-orchitis. As in civilian practice, nonrenal diagnoses are frequently demonstrated on MDCT of the kidneys, ureters, and bladder.
Radiologists are also diagnosing ovarian cysts, pelvic inflammatory disease, acute cholecystitis, and pregnancy in women serving in war zones.
"The ability to offer definitive imaging in the operation environment for disease or nonbattlefield injury allows troops to be managed locally and stay on deployment rather than having to be repatriated for diagnostic workup," Graham wrote.
Plain film and ultrasound are useful, but MDCT has made all the difference in terms of diagnosing battlefield trauma.
"The days of radiologists not deploying to operational theatres are hard to imagine," Graham concluded. "Remote reporting of MDCT images is too slow and is not fit for purpose with the operational tempo we see today. Radiology, radiologists, and radiographers are firmly in the center of battlefield trauma care, and are a vital component of the deployed clinical team."