Postmortem CT angiography combined with image-guided biopsy can nearly always determine the cause of death in patients who succumb after acute chest pain, a question that has often gone unanswered, according to a Swiss study published in Radiology.
Compared to traditional autopsy, CT in combination with minimally invasive biopsy identified the cause of death in 95% of patients examined, a team from Bern, Switzerland, reported. CT and MRI can enhance the practice of manual autopsy and in many cases even replace it, the group concluded.
Acute chest pain is related to various cardiovascular diseases that can lead to sudden death in about 1 million patients a year in the U.S. However, the incidence of death from noncardiac diseases is unknown because autopsies are not systematically performed, according to the researchers.
Information from CT has helped improve diagnosis in a wide range of chest diseases, including pulmonary embolism, aortic dissection, acute coronary syndrome, and lung cancer. Yet the standard postmortem exam has not changed in centuries.
 |
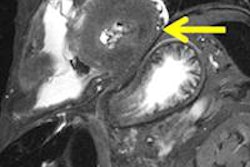
| 3D volume rendering of heart shows left anterior descending (LAD) coronary artery with high-grade (approximately 90%) stenosis (arrow) in proximal segment. Additionally, there is eccentric hypertrophy of left ventricle. All images republished with permission of RSNA from May 8, 2012, doi: 10.1148/radiol.12092415. |
"To enhance the customary and partially restricted approach of manual autopsy, the introduction of multidetector CT and magnetic resonance imaging represents an innovation in the field of forensic pathology, as these methods act as valuable diagnostic adjuncts or even potential replacements for traditional autopsy," wrote Dr. Steffen Ross, Dr. Michael Thali, and colleagues from University of Bern and University of Zurich (Radiology, May 8, 2012).
The study aimed to assess the utility of minimally invasive postmortem CT and image-guided tissue biopsy of the myocardium and lungs to determine the cause of death in patients who died after acute chest pain, with autopsy as the reference standard.
Initial experiments in postmortem CT autopsy have focused on bones and air-containing structures using unenhanced CT, as there was no feasible method of applying contrast media, but the situation has changed.
"During recent years, further attempts to establish a minimally invasive approach by using various contrast medium mixtures (e.g., iodized oil and a diluting alkane or polyethylene glycol with iodinated contrast medium) with subsequent postmortem CT angiography of the whole body have led to promising results," the authors wrote.
Meanwhile, research groups have used postmortem biopsy procedures as an alternative to tissue sampling during autopsy.
 3D volume rendering of thoracoabdominal aorta shows Stanford type A aortic dissection with a small cleft of the adventitia and a 7-mm tear in the intima directly arising from the aortic root and extending into the ostium of the left coronary artery, resulting in hematopericardium. The extravasation (dotted circles) indicates a hemorrhage into the pericardium that led to a fatal tamponade of approximately 750 mL. Note the good delineation of the false (arrowhead) and true (arrow) lumens.
3D volume rendering of thoracoabdominal aorta shows Stanford type A aortic dissection with a small cleft of the adventitia and a 7-mm tear in the intima directly arising from the aortic root and extending into the ostium of the left coronary artery, resulting in hematopericardium. The extravasation (dotted circles) indicates a hemorrhage into the pericardium that led to a fatal tamponade of approximately 750 mL. Note the good delineation of the false (arrowhead) and true (arrow) lumens.
In the current study, Ross and colleagues examined 20 corpses (4 female, 16 male; age, 15-80 years); all of the patients had reported acute chest pain. The researchers used whole-body CT angiography and image-guided biopsy, including three biopsies of the myocardium and a single biopsy of bilateral central lung tissue.
After an initial analysis of the cross-sectional images, the group performed additional biopsies of thrombi, followed by traditional autopsy with sampling of histologic specimens. Finally, histologic and autopsy reports were compared with the postmortem CT angiography and image-guided biopsy findings.
Postmortem imaging was performed with a six-detector-row CT scanner (Somatom Emotion 6, Siemens Healthcare) using a triphasic protocol (including unenhanced, arterial, and venous phases) from the head to the pelvis.
Supine unenhanced imaging was followed by contrast administration and a second scan; the cadaver was then turned to the prone position to ensure "filling of all coronary arteries and to overcome gravity effects in the vessel lumen," the group wrote. After at least 15 minutes, an additional bolus of contrast was injected and the cadaver was rescanned in the supine position.
Unenhanced CT was performed at 130 kV and 160 mAs using 1-mm collimation. Cardiac imaging was performed using a section thickness of 0.5 mm, 110 kV, and 250 mAs.
Two radiologists experienced in forensic imaging reviewed all images on a workstation (Leonardo, syngo 2008C MultiModality Workplace, Siemens), and PACS (Sectra) was used for review of images reconstructed with section thicknesses of 5 mm, 1.25 mm, and 0.625 mm, using a reconstruction interval of half the section thickness.
In 19 of the 20 cadavers, findings at postmortem CT angiography in combination with CT-guided biopsy validated the cause of death found at traditional autopsy. In one cadaver, early myocardial infarction of the papillary muscles had been missed. Cohen's kappa coefficient was 0.94. In seven of the 20 cadavers, CT-guided biopsy provided additional histopathologic information that substantiated the final diagnosis of the cause of death.
The results showed four instances of pulmonary embolism, three aortic dissections (all Stanford type A), three myocardial infarctions, three instances of fresh coronary thrombosis, three cases of obstructive coronary artery disease, one ruptured ulcer of the ascending aorta, one ruptured aneurysm of the right subclavian artery, one case of myocarditis, and one pulmonary malignancy with pulmonary artery erosion.
In each case of cardiac disease, "postmortem CT angiography with the cadavers in the supine position enabled complete opacification of the lumens of the major left coronary arteries and their side branches into their distal parts with diagnostic quality," Ross and colleagues wrote. "Most notably, the right coronary artery showed complete contrast material filling because of changed gravity effects after the corpse was turned to the prone position, with complete opacification of the vascular lumen in all cases."
Similarly, in the three Stanford type A aortic dissections, arterial contrast material injection "allowed distinct identification between the true and false lumens and of the extension of the dissection, including entry and re-entry," the group noted.
In the pulmonary arteries, CT angiography after venous injection to display the pulmonary arteries showed segmental and subsegmental filling defects in 10 cadavers.
"In one case, myocardial biopsy showed contraction band necroses as a sign of a fresh myocardial infarction," they wrote. "Nevertheless, one case of early myocardial infarction could only be detected in the histologic specimen gathered during autopsy because of its localization in the papillary muscles, which were not sampled for biopsy."
The missed acute myocardial infarction at CT-guided biopsy could have been avoided if the papillary muscle had been included in the standard biopsy protocol, they noted.
Finally, the histopathologic diagnoses of standardized CT-guided biopsy samples of the myocardium were concordant with tissue specimens gathered during autopsy.
"Postmortem CT angiography enabled the depiction of cardiac findings like coronary artery disease and coronary thrombosis and the evaluation of cardiac bypasses in situ," they wrote. "Image-guided biopsy provided substantial additional information about the myocardium in cases of myocarditis and myocardial infarction, and imaging without biopsy would not have been able to help identify these diseases."
The depiction of noncardiac diseases such as aortic dissection, pulmonary embolism, and nontraumatic vascular rupture showed complete concordance in all subjects.
"The results of this study clearly show the potential of postmortem CT angiography to change the paradigm in the investigation of the cause of death by introducing a minimally invasive technique for postmortem examination," Ross and colleagues concluded.
"Imaging and biopsy may augment both clinical and forensic postmortem examinations and serve as a viable compromise or even a substitute for traditional autopsy," they continued. "Furthermore, the data acquired by imaging can be re-evaluated at any point in time and are fully reproducible for future research and/or counterexpert examinations."