Researchers from Italy and Spain have found that communication affects whether women will return for their annual mammogram, and, similarly, a false-positive result deters them from coming back. The findings were published in this month's issue of the European Journal of Public Health.
In the study out of Italy, Livia Giordano from the Center for Cancer Prevention in Turin and colleagues performed a randomized trial of different methods of involving and informing women about mammography screening (Eur J Public Health, June 2012, Vol. 22:3, pp. 413-418).
They compared the delivery of standard information on mammography with additional information such as side effects and limitations. With the secondary group, they analyzed the effect of different socio-demographic and organizational determinants on mammography screening participation. Though the organized Turin breast cancer screening service invites all women between the ages of 50 and 69 to participate, the authors invited younger women because mammography screening in those younger than 50 is controversial.
"The balance between its advantages and disadvantages is one of the most critical matters," wrote Giordano, who is president of the Gruppo Italiano Screening Mammografico. "How to transmit information, the degree of detail, and, above all, the effect on women's participation are issues that screening operators are debating for a long time. In younger women, the matter of communication becomes even more a priority, still greater if compared with older women, given the uncertainty of the efficacy of mammography screening in this age group."
The study included 5,744 women ages 40 to 45 who were randomly assigned letters with the following:
- Group 1: A prefixed appointment plus standard leaflet
- Group 2: A prefixed appointment plus a more comprehensive booklet
- Group 3: A prefixed appointment plus the offer of a counseling session
- Group 4: No appointment but a letter inviting women to contact the center to receive additional information
After exclusion criteria, 5,360 women participated in the study. Participation rates following the first contact were 36.5%, 39.9%, 35.8%, and 16.5%, respectively, for each group. The rates increased to 40.9%, 43.6%, 40.1%, and 35.1%, respectively, after reminder letters. Women receiving more complete information had a higher uptake, although it was not statistically significant.
"These results suggest that providing a larger amount of written information, broadening on screening procedures, benefits, and limits of the test, does not influence participation," the authors noted.
The researchers do acknowledge, however, that the presence of an organized screening program in the area that has been active for a long time and is well-known by the population may partly justify the lack of a significant difference between the different communication strategies.
They also found participation was higher among married, higher-educated, and white-collar working women, as well as those born in Northern and Central Italy, women who lived closer to the screening unit, and those with a female collaborative doctor.
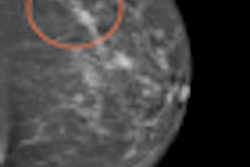
Effect of false positives
Learning more or less about screening doesn't affect the attendance rate, but getting a false-positive result does, according to research by Dr. Dolores álamo-Junquera from Servei d'Epidemiologia i Avaluació, Hospital del Mar - Parc de Salut Mar in Barcelona and colleagues (Eur J Public Health, Vol. 22:3, pp. 404-408).
More than 1.3 million women between the ages of 44 and 67 were initially screened for breast cancer from 1990 to 2004 in their study. Of the 120,800 women with a false-positive screening mammogram, 78.3% returned for a subsequent screening mammogram, compared with 81.9% of those with a negative result, the researchers found. In addition, the likelihood was even lower for those who had undergone invasive additional tests (odds ratio = 0.56; 95% confidence interval: 0.53-0.59).
"Uncertainty about test results may produce more worries than a negative or clearly positive result," the authors wrote. "This uncertainty is produced during the screening process while the woman is waiting for the results of additional tests performed as a consequence of a non-negative mammogram."
The results also shows the difference between the U.S. and Europe -- in the U.S. there is a higher reattendance among women with a false-positive screening mammogram, which could be explained by a contrast in breast screening policies between the U.S. and Europe.
Reattendance was also lower for women older than 60, possibly because these women have less interest in the screening program or they switched to the private health sector after the initial screening. Similarly, reattendance of subsequent screening mammograms was lower for menopausal women.
"A better understanding of factors affecting reattendance is fundamental to increase the impact of breast cancer screening," the authors wrote. "The effect on reattendance of interventions to reduce anxiety, such as involvement of primary care physicians or the information provided to women about breast cancer and screening, should be evaluated."
The study had some limitations:
- In some regions, some women use private medicine for gynecological tests.
- The researchers could not determine whether the women who decided against attending the second screening had mammograms performed outside the program.
- Not all regional mammographic screening programs in Spain were included and, consequently, although almost half of the target population was covered, extrapolation of the results could be problematic.
- No information on the educational level of the screening participants was known.
Nonetheless, the authors maintain the results could be used to improve the screening process and increase women's compliance with these programs.