Dual-source CT is as accurate as MRI, and better than echo, for evaluating the left ventriculum (LV) years after patients receive transplanted hearts, according to a joint Spanish and Italian study in the European Journal of Radiology that compared dual-source CT (DSCT) and echocardiography with cardiac MRI (CMR).
DSCT was closely tied to CMR measurements, the study team found, but echocardiography was too imprecise to compete with either advanced modality.
Among the 25 patients who had undergone heart transplant procedures years earlier, contrast-enhanced echo led to significant underestimation of left ventricular volumes and overestimation of ejection fraction compared to both DSCT and CMR.
"DSCT allows estimating left ventricular volumes and ejection fraction similarly to CMR in orthotopic heart transplant recipients," wrote Dr. Maria Arraiza from the department of radiology at the University of Navarro in Pamplona, Spain, along with colleagues from Pamplona and the University of Rome.
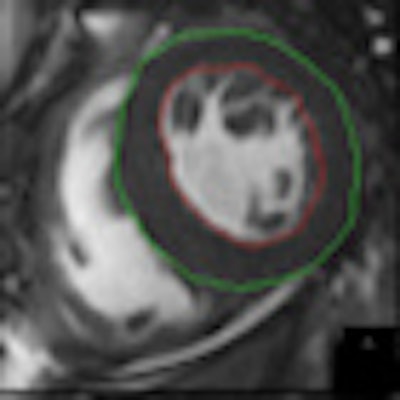
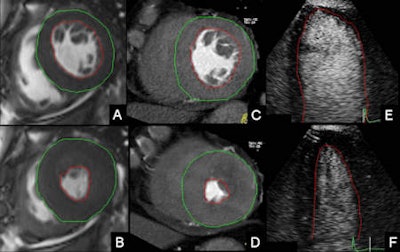 Left ventricular (LV) manual contour tracing for the assessment of LV parameters in cardiac MRI (CMR), cardiac dual-source CT (DSCT) and 2D contrast-enhanced echocardiography (CE echo). A, B: CMR short-axis views. C, D: Cardiac DSCT short-axis views. E, F: Two-dimensional CE echo apical four-chamber views. A, C, E: End diastole. B, D, F: End systole. Images courtesy of Dr. Maria Arraiza.
Left ventricular (LV) manual contour tracing for the assessment of LV parameters in cardiac MRI (CMR), cardiac dual-source CT (DSCT) and 2D contrast-enhanced echocardiography (CE echo). A, B: CMR short-axis views. C, D: Cardiac DSCT short-axis views. E, F: Two-dimensional CE echo apical four-chamber views. A, C, E: End diastole. B, D, F: End systole. Images courtesy of Dr. Maria Arraiza.Evaluation of patients who have undergone heart transplants requires early detection of graft vasculopathy and accurate assessment of cardiac volumes, function, and mass so as to improve graft outcomes and increase patient survival, the study team noted in an article-in-press published online on 4 May.
Two-dimensional echocardiography has traditionally been used for such assessment, but its lack of reproducibility and accuracy has been only partly corrected by the use of contrast enhancement, leaving CMR as the reference standard, while CT has emerged as a potential contender that has not been adequately examined.
"This study aimed to expand previous preliminary and limited clinical observations about the ability of DSCT and 2D contrast-enhanced transthoracic echocardiography to estimate allograft function in orthotopic heart transplant recipients," they wrote.
They examined 25 consecutive heart transplant recipients (20 men, mean age 62.7 years, mean BMI 26.5) who had undergone heart transplants a mean 8.1 ± 5.9 years earlier.
Coronary CT angiography with retrospective gating was performed on a DSCT system (Somatom Definition, Siemens Healthcare) at 120 kV, 350-400 reference mAs per rotation using automated tube current modulation (Caredose 4D, Siemens Healthcare), and 0.6-mm collimation. Retrospective ECG-gating was used with full tube current between 30% and 80% of the cardiac cycle. Iodinated contrast (70 mL, Iomeron, Bracco Diagnostics) was injected followed by 50 mL saline using a dual-syringe injector. From the raw image data, 8-mm section thickness double oblique short-axis images were retrospectively reconstructed in 5% steps throughout the cardiac cycle.
CMR studies were performed on a 1.5-tesla system (Magnetom Symphony TIM, Siemens Healthcare) equipped with quantum gradients, using a four-element phased-array surface coil and retrospective ECG synchronization. Steady-state free precession (SSFP) short-axis orientation cine images were acquired at TR 2.89 msec, TE 1.3 msec.
For the echo images, contrast-enhanced echocardiography studies (iE33 ultrasound system and S5 transducer, Philips Healthcare) were performed using baseline two- and four-chamber apical views and standard parasternal long- and short-axis views.
Two readers working independently analyzed the DSCT, echocardiography, and CMR images in random order, blinded to the results of the other imaging modalities.
The results showed no statistical difference between left ventricular volumes in DSCT and CMR. The mean end-diastolic volume (EDV), end-systolic volume (ESV), and stroke volume (SV) at DSCT were all very similar to the CMR assessments (p > 0.5), Arraiza and colleagues reported.
The mean ejection fraction didn't differ significantly between DSCT and CMR even when the difference was very close to statistical significance (p = 0.051), and there was good correlation between DSCT and CMR for left ventricular measurements (r ≥ 0.77; p < 0.0001).
Comparison of left ventricular volumes and function per DSCT and MRI
|
However, left ventricular measurements were statistically different when echocardiography was compared with DSCT and CMR, they said, with echo showing a lower mean EDV (86.7 ± 24.2 mL), ESV (29.4 ± 18.7), SV 57.5 ± 14.1 mL), and a higher mean ejection fraction (EF) than both DSCT and CMR (p <0.05).
"The main finding of the present study is that DSCT allows estimating left ventricular volumes and ejection fraction similarly to CMR in orthotopic heart transplant recipients," Arraiza and colleagues wrote. "Evaluation of these parameters with [contrast-enhanced echocardiography] results in significant underestimation of left ventricular volumes and overestimation of left ventricular ejection fraction."
Agreement and reliability for left ventricular measurements were notably higher between cross-sectional imaging techniques compared with the agreement observed between echo, and either DSCT or CMR.
In transplant patients, multidetector-row CT (MDCT) and particularly DSCT "may provide diagnostic image quality examinations that may enable ruling out cardiac allograft vasculopathy," they wrote. "In fact, CT has been suggested as a noninvasive tool for monitoring heart transplant patients."
However, there has been limited evidence regarding the validity of CT to quantify cardiac function in heart transplant recipients. Studies have focused on evaluating left ventricular function with CT, and the results have been mixed, particularly in individuals with high resting heart rates, they stated.
The uneven performance in fast hearts may be due to insufficient temporal resolution of conventional MDCT systems to achieve accurate left ventricular measurements in such conditions, but here, DSCT technology with its higher temporal resolution may be the solution.
In line with recent studies assessing left ventricular function with DSCT, "this study demonstrates that the superior temporal resolution of DSCT systems (83 msec) turns out into more accurate estimation of left ventricular volumes," Azairra and colleagues wrote.
Moreover, DSCT seems to be reliable to assess left ventricular ejection fraction as well, even when the differences turn out to be very close to statistical significance.
"Nevertheless, in clinical practice, DSCT should be used for the sole analysis of cardiac function only in cases of inadequate images from other noninvasive methods and not as a first-line imaging modality," they wrote.
As for limitations, the study population was limited, and different numbers of phases were used in CT and MRI, which might have caused inaccuracies in identifying end systole and end diastole.
Newer cardiac CT acquisition techniques based on prospective ECG gating may be able to perform functional studies with significantly reduced radiation, and iterative reconstruction could cut the dose even further, according to the authors.
"Cardiac DSCT may allow comprehensive assessment of the heart in transplant recipients undergoing coronary DSCT imaging by allowing it to rule out cardiac allograft vasculopathy and quantify left ventricular functional parameters without additional contrast administration or radiation exposure," they concluded.