MRI may be the gold standard for evaluation and follow-up of heart transplant patients, but multidetector CT (MDCT) can be well-suited to the conditions of the transplanted heart that evolve in the days and months following surgery.
In a study presented at this month's European Congress of Radiology (ECR), researchers from the University of Rome La Sapienza compared MDCT with MRI and echocardiography and found good correlation of most functional parameters with MRI, and moderately good correlation with echo. MDCT has slightly lower temporal resolution than MRI, but its ability to quickly evaluate the coronary arteries is a big advantage in follow-up care, the group reported.
The needs of cardiac evaluation for transplant patients evolve over time after surgery, but the need for accurate left ventricular (LV) function assessment is critical, said Dr. Valentina Silvestri.
"Cardiac morbidity and mortality are strictly correlated to LV functional parameters, especially in heart transplant patients," she said, noting that the accuracy of the modality measuring these parameters is particularly important:
In the first month after surgery, clinicians are looking for postoperative complications, acute graft failure, early acute rejection, arrhythmia, and adverse events from the immunosuppressive drugs.
During the first year after surgery, doctors are on the lookout for acute rejection as well as infections from cytomegalovirus (CMV), Candida, and the like.
After the first year, the diagnostic focus shifts to coronary allograft vasculopathy, neoformations, late acute rejection, and again, adverse events from the immunosuppressive medication. The later emergence of vasculopathy "has to do with the rapid progression of atherosclerosis, which will represent the major limitation to long-term prognosis of these patients several years after surgery," Silvestri said.
For all of these potential complications, MDCT's imaging capabilities make it a good fit, if it's sufficiently accurate, she said.
"What we suggest is to introduce MDCT as a global diagnostic investigation to assess both the coronary arteries and cardiac function," said Silvestri, adding that this study focused on the critical topic of MDCT in LV functional assessment. "We compared MDCT with echo and cardiac magnetic resonance (CMR) -- that is the gold standard technique. All techniques were performed on the same day within a very short temporal window to avoid bias due to hemodynamic and functional changes."
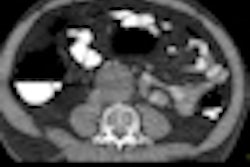
The study included 16 heart-transplant patients with normal sinus rhythm who underwent 64-detector-row retrospective ECG-gated MDCT (LightSpeed VCT, GE Healthcare) with tube current modulation, comparing the results to CMR (1.5-tesla scanner, 8-16 short-axis steady-state free-precession images) and echocardiography (3 mHz probe, apical view measurements). All exams were performed on the same day for each patient.
Two expert readers blinded to the results of other modalities independently evaluated LV function at MDCT in terms of ejection fraction (EF), end-diastolic volume (EDV), end-systolic volume (ESV), stroke volume (SV), cardiac output (CO), and mass of the left ventriculum using dedicated software on a workstation (TeraRecon), comparing the results to CMR and echocardiography. MDCT interobserver agreement was measured and heart rate was measured during all of the exams, and no beta-blockers were used.
"The ejection-fraction results were lower for MDCT versus MRI, while end-diastolic volume, systolic volume, and stroke volume were statistically significantly higher for MDCT, but with a high correlation coefficient," she said. "At the same time, for cardiac output and LV mass interobserver agreement was high."
LV functional parameters for MDCT vs. CMR and echocardiography
|
The MDCT versus echo results were less well correlated, according to Silvestri, though the Bland-Altman analysis shows a fair agreement for ejection fraction for cardiac output and mass, and good agreement for end diastolic volumes and end-systolic volumes.
The results are similar to those reported in the literature, with one important difference being that in prior studies all the exams weren't all performed on the same day. Also notable were significant differences in heart rates between modalities. Differences in beta blockers may have contributed to differences in LV volume values, she said, as heart rate and LV values are inversely proportional. In addition, exam conditions were somewhat different. MDCT was performed in a single breathhold while CMR was performed with repeated expiratory breathholds, and echocardiography in both expiratory and inspiratory phases.
Study limitations include a small population due to the uniqueness of the study pathology, as well as CT's reduced temporal resolution versus MRI and MDCT's radiation dose.
"Our conclusion is that MDCT is able to assess heart transplant patients with relatively good agreement with MR in relation to end-diastolic volumes, end-systolic volumes, stroke volumes, cardiac output, and mass," Silvestri said. "MDCT is also able to perform LV assessment within a global diagnostic approach including coronary artery evaluation in a fast exam."
MDCT's results seem sufficiently reproducible to consider its use in the follow-up of transplant patients, and to support therapeutic strategies.
Larger studies are needed to confirm these results, which are likely to improve in the future with new scanner models featuring higher temporal resolution and lower radiation doses, she concluded.