
When three outbreaks of tularemia occurred in northeastern Turkey in 2004 and 2005, Europe was stunned at the chilling prospect of a little-known infectious disease that can spread so rapidly from animals to humans. Now radiologists are using MRI to provide valuable clinical information in complex cases.
Tularemia is an acute bacterial infectious disease caused by a pleomorphic, nonmobile, noncapsulated, small gram-negative coccobacillus and zoonotic bacterium, Francisella tularensis. F. tularensis is a highly infectious pathogenic bacterium and requires inoculation or inhalation of as few as 10 organisms to cause disease. It is also used by terrorists as a biological weapon, according to Dr. Safiye Gürel and Dr. Kamil Gürel, from the department of radiology at the Abant Izzet Baysal University School of Medicine in Bolu, Turkey.
This zoonotic bacteria has infected a wide range of wild animals, including rabbits, hares, squirrels, muskrats, moles, skunks, beavers, and deer, as well some domestic animals such as sheep, cattle, and cats. Birds, amphibians, and invertebrates (ticks, deer flies, and mosquitoes) also have been infected. Transmission to humans is by insect vectors, handling or ingestion of infected animal tissues, inhalation of infectious aerosol, and consumption of contaminated drinking water.
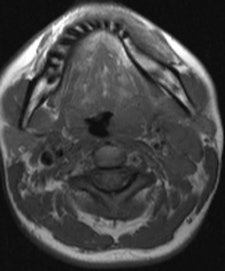
 A 30-year-old woman suffering from oropharyngeal tularemia. She presented with painful left-sided cervical mass. Hypertrophic left palatine tonsil (arrow), narrowing oropharynx, isointense on T1-weighted and hyperintense on T2-weighted images compared with striated muscle with homogeneous contrast enhancement is seen on axial TSE T1-weighted (left), short tau inversion recovery (right). All images courtesy of Dr. Safiye Gürel.
A 30-year-old woman suffering from oropharyngeal tularemia. She presented with painful left-sided cervical mass. Hypertrophic left palatine tonsil (arrow), narrowing oropharynx, isointense on T1-weighted and hyperintense on T2-weighted images compared with striated muscle with homogeneous contrast enhancement is seen on axial TSE T1-weighted (left), short tau inversion recovery (right). All images courtesy of Dr. Safiye Gürel."Radiologists should be aware of tularemia, especially in endemic areas. Usually unilateral, or bilateral in advanced cases, lymphadenopathies associated with hypertrophied lymphoid tissue are the most suspicious findings from a radiological point of view," Dr. Safiye Gürel told AuntMinnieEurope.com. "In advanced cases, the addition or presence of accompanying significant necrosis in lymph nodes and painful soft-tissue swelling is helpful in differentiating a case from tuberculosis or malignancy."
Most cases occur between June and September, when arthropod-borne transmission is most common. In the U.S., cases are mostly sporadic or occur in small clusters, while in Europe and Asia, waterborne, arthropod-borne, and airborne outbreaks can involve hundreds of people. The incidence is not known, but the disease is often unrecognized and often underreported, they noted in a presentation at the RSNA 2011 congress in Chicago.

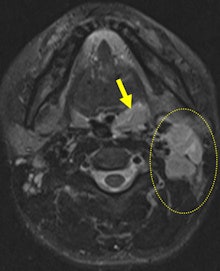
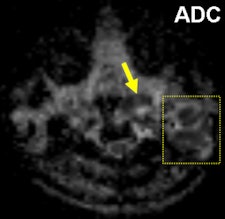 The same patient as seen on postcontrast fat-saturated T1 weighted (left), respectively. Left-sided peripherally enhanced, mostly necrotic, lymphadenopathies (dashed circle) are present on level 2 on axial short tau inversion-recovery and axial postcontrast fat-saturated T1-weighted images. Accompanying minimal signal intensity change and increased thickness of neighboring soft-tissue planes are seen as well. Remarkable restriction of diffusion is illustrated within lyphadenopathies and left palatine tonsil (ADC = 0.82 mm/sn2) (right).
The same patient as seen on postcontrast fat-saturated T1 weighted (left), respectively. Left-sided peripherally enhanced, mostly necrotic, lymphadenopathies (dashed circle) are present on level 2 on axial short tau inversion-recovery and axial postcontrast fat-saturated T1-weighted images. Accompanying minimal signal intensity change and increased thickness of neighboring soft-tissue planes are seen as well. Remarkable restriction of diffusion is illustrated within lyphadenopathies and left palatine tonsil (ADC = 0.82 mm/sn2) (right).The clinical manifestation of tularemia may vary from asymptomatic illness to fulminant toxemia with septic shock, and presentation is dependent on the organism and the route of transmission. Tularemia is traditionally classified into the following clinical types, depending on the route of transmission: ulceroglandular (80%), glandular (15%), oropharyngeal (less than 5%), oculoglandular (1%), typhoidal (less than 1%), and pneumonic (less than 1%). The main symptoms and signs of both the ulceroglandular and glandular form are seen in the head and neck region.
In Turkey, oropharyngeal tularemia is the most common type, and the predominant symptoms are fever and severe throat pain. In the 2004 and 2005 outbreaks, the clinical manifestations were similar to those of oropharyngeal tularemia, and water contamination was thought to be the likely source, Safiye Gürel stated. Exudative pharyngitis or tonsillitis with oral ulcers and unilateral cervical, preauricular, and retropharyngeal lymphadenopathy are the main findings. Occasionally, this form presents with bilateral involvement of lymph nodes or abscess formation.

| Tularemia is a zoonosis, or an infection that can be spread from animals to humans. It is caused by the bacterium Francisella tularensis, which can infect many animals, especially rabbits, hares, and small rodents |
"The lesion consists of a granulomatous reaction that in some cases may have a frankly tuberculoid appearance, in particular in the more chronic lesions, but the necrosis is more liquefactive than caseous. The widespread necrosis with polymorphs, lymphocytes, and multinucleated giant cells is surrounded by radially arranged epithelioid cells and fibrosis," he explained.
On MRI, oropharyngeal tularemia mostly presents with unilateral lymphadenopathy and associated oropharyngeal lymphoid tissue hypertrophy. A spectrum of homogeneous to inhomogeneous, and/or peripheral enhancement is parallel to development of central necrosis in the lymph nodes. Accompanying increased signal intensity occurs on T2-weighted images, and contrast enhancement of neighboring soft-tissue planes may be noted, especially in cases of suppuration. Restricted diffusion and an apparent diffusion coefficient (ADC) ranging from 0.5-1.05 mm/sn2 also are evident.
The main weakness of MRI is that its findings are nonspecific. Furthermore, both conventional MRI and diffusion-weighted imaging findings (ADC values) overlap with other granulomatous infections such as cat scratch disease and some malignant neoplasms such as squamous cell carcinoma, the researchers found.
Oropharyngeal tularemia should be considered in patients with a sore throat -- with or without an accompanying tender head and neck mass -- that does not respond to beta-lactam antibiotics and demonstrates necrotic lymphadenopathy and/or oropharyngeal lymphoid tissue hypertrophy with restricted diffusion in an MRI examination, particularly in endemic areas, they concluded.



















