
These days, multidetector-row CT (MDCT) is producing vast quantities of 3D and 4D data for diagnostic and interventional use. But for all its multidimensionality, most of the output is still served up on a flat screen. That could be changing with a process called "rapid prototyping" that creates physical models from imaging data.
Rapid prototyping is a widely used industrial process that converts a virtual 3D image into a physical 3D model using a special printer. Israeli radiologists have found that rapid prototyping could have medical uses by putting precise models of patient anatomy in surgeons' hands.
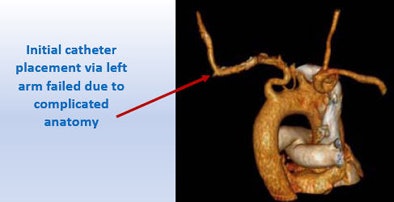
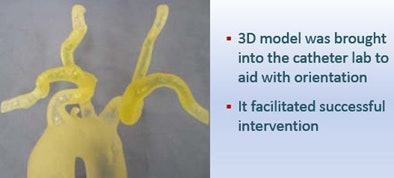
In a presentation at the 2011 meeting of the International Society for Computed Tomography (ISCT) in San Francisco, Dr. Jacob Sosna explained how the tactile models simplify complex cases and improve the planning of interventional procedures.
Rapid prototyping can be seen as a logical extension of traditional image postprocessing techniques performed in a 3D lab to make CT images easier to interpret, said Sosna, who is an associate professor of radiology and director of the 3D lab at Hadassah Hebrew University in Jerusalem.
"Rapid prototyping allows us to take 3D data and look at it in another dimension -- actually, a fifth dimension -- that we can't get just using computer models," he said.
 |
| A 23-year-old man presented with a dramatic fracture of the right scapula from an elevator accident (above). Use of a 3D model allowed surgeons to actually cut the scapula model and carefully design the plates to be implanted (below) before the patient was taken to surgery, leading to a shorter operation time and a successful outcome (bottom image). All images courtesy of Dr. Jacob Sosna. |
 |
 |
Transition to medical imaging
Neither the techniques nor the printers that enable rapid prototyping are new, Sosna said. The approach is a mainstay in industrial applications, where new components can be modeled quickly for evaluation before they reach the production stage.
In medical imaging, rapid prototyping improves the ability of surgeons to understand complex anatomy, and it gives them an opportunity for hands-on interaction, Sosna said.
In Sosna's 3D lab, the prototyping is performed by converting DICOM image data into another format, SDL, and sending the data to a special 3D printer (Eden260V, Objet). The printer applies layers of a photopolymer resin via a high-resolution inkjet, then cures the sculpture using an ultraviolet light source.
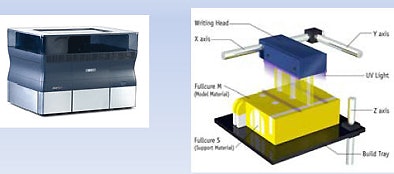 |
| The 3D printer applies layers of a photopolymer resin via a high-resolution inkjet at about 1 cm per hour, curing the sculpture via ultraviolet light. |
"Photo-quality resin is applied via high-resolution injection and cure," he said. "It's like your printer at home, but when you inject the printing material it becomes stronger. The scanner we use prints at about 1 cm per hour, so if the anatomy is 6-mm long it takes about six hours." At that speed, "it's not intended for the emergency department, but it can be used in everyday practice."
Rapid prototyping offers an added dimension that cannot be realized by simply looking at computer models on a flat screen, Sosna said.
"It allows surgeons an improved ability to understand complex anatomy and an opportunity for hands-on interaction when they perform the procedure," he said. "It may improve outcomes in complex cases and reduce operating room time, and we have data supporting that. Finally, it reduces blood loss and wound exposure and reduces the need for anesthesia since surgery becomes shorter."
New applications are emerging in oral surgery, neurosurgery, vascular surgery, cardiology, and orthopedic surgery, he said.
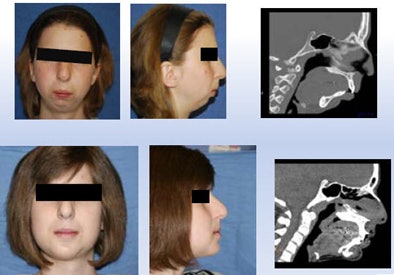 |
| Above, girl with severe mandibular hypoplasia (top row, preprocedure; bottom row, postprocedure) benefited from the surgeon's ability to work with a precise model (below). |
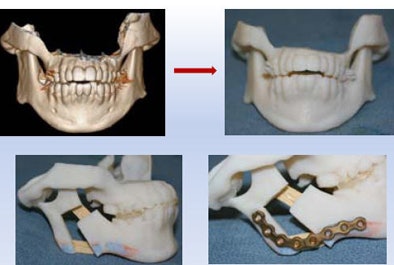 |
The surgeon was able to cut the mandible model and precisely fashion the prostheses, e.g., the plate that was attached, leading to a good outcome that was functionally as well as aesthetically optimal, Sosna said.
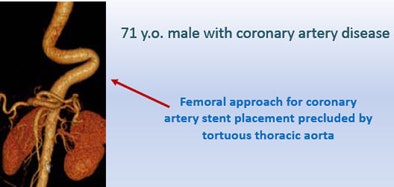 |
| Treatment of a 71-year-old man with coronary artery disease was complicated by the patient's tortuous thoracic aorta. The surgeon's ability to practice implantation of a new aortic valve on a 3D model led to successful surgery. |
 |
 |
Rapid 3D prototyping offers a completely new dimension to the image postprocessing toolkit, one that can't be replaced by computer models and is destined to be an important technique in selected cases, Sosna said.
"I don't say we can use it in every case, but at least for complex anatomical cases, even neurosurgery, it can be used and is quite well-accepted," he said.



















