MR-guided biopsies can produce valuable results, but often they are time-consuming and expensive. To make them a more realistic clinical proposition, it is vital to cut the preparation time, obtain fewer image acquisitions, and involve experienced interventional radiologists, researchers from the University of Tübingen in Germany have reported in an online first article published on 30 September by European Radiology.
MR-guided biopsies can be useful for diagnosing malignancies in musculoskeletal and hepatic lesions, particularly in cases in which CT and ultrasound-guided methods are unsuccessful. This is due to MR's high soft-tissue contrast, the option to adjust the imaging plane to the needle trajectory, the good visualization of vessels without the use of contrast agents, and the lack of ionizing radiation, the authors stated. However, the major drawbacks are the high cost of a specialized interventional MR unit or MR-compatible biopsy systems, plus the length of the procedure and the need to occupy an MRI suite for a significant length of time.
The group, led by Dr. Rüdiger Hoffmann from the department of diagnostic and interventional radiology, assessed the accuracy and duration of MR-guided biopsies of hepatic and soft-tissue lesions in clinical routine by retrospectively reviewing the 38 most recent biopsies where MR guidance was chosen for intervention. As a result of the study, they have now introduced a defined pattern of sequences for biopsies and have tried to reduce the procedure time, Hoffmann noted in an email response to AuntMinnieEurope.com.

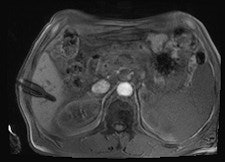
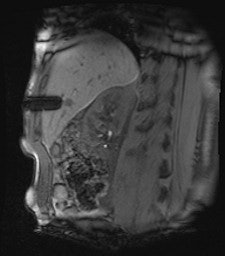
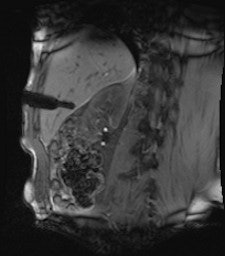
 A 50-year-old man with history of pancreatic carcinoma underwent a CT-guided biopsy (above), which was nonconclusive (pathology result: normal liver tissue). Three weeks later, an MR-guided biopsy (below) was performed, and the biopsy revealed a cavernous hemangioma. Images courtesy of Dr. Rüdiger Hoffmann.
A 50-year-old man with history of pancreatic carcinoma underwent a CT-guided biopsy (above), which was nonconclusive (pathology result: normal liver tissue). Three weeks later, an MR-guided biopsy (below) was performed, and the biopsy revealed a cavernous hemangioma. Images courtesy of Dr. Rüdiger Hoffmann.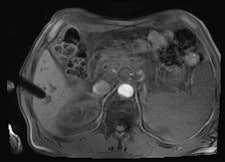
At the University of Tübingen, ultrasound and CT are the preferred guidance techniques for biopsies, and MR-guidance is reserved for special conditions. The study included a total of 15 (39%) female patients and 23 (61%) male patients, with a mean age of 51.8 years, ranging from 7 months to 78 years.
Documentation about the reason for MR guidance was recorded in 15 cases, the authors wrote. In five cases, a previous CT- or US-guided biopsy was inconclusive. In two cases, the target could not be adequately demonstrated by CT due to the low contrast of the lesion compared with surrounding tissues. In one patient with a joint prosthesis, streak artifacts limited the use of CT. In five patients younger than age 30, MR guidance was chosen to avoid ionizing radiation. In two patients with suspicion of inflammatory muscular disease, the aimed muscle edema was only sufficiently visible under MR guidance.
All procedures were performed using a wide-bore 1.5-tesla MR system (Magnetom Espree, Siemens Healthcare). A radiofrequency-shielded liquid-crystal display monitor was installed next to the magnet for real-time monitoring. During the procedures, imaging was performed with the use of a flexible four-channel body-array surface coil and a loop coil, and biopsies were performed with MR-compatible puncture needles. To obtain the specimen, an MR-compatible biopsy device (MRI Biopsy Handy, Somatex Medical Technologies) was used in 36 cases. After placing the MRI-compatible puncture needle in the magnet, two intramuscular biopsies were performed using a non-MR-compatible spring-loaded biopsy gun (ASAP, Boston Scientific) outside the magnet. During the biopsy, vital parameters were monitored using an MR-compatible patient monitor (Invivo 4500 MRI, Invivo Research).
In nine cases -- eight soft-tissue, one liver -- MR fluoroscopy was used to define the entry site, and the physician used a fingertip or water-filled syringe as a marker. In 29 cases -- 11 soft-tissue, 18 liver -- a marker capsule (Adalat, Bayer) was affixed to the supposed entry side with adhesive tape, and the position was corrected after application of conventional sequences. After sterile draping, administration of local anesthesia and skin incision, an MR-compatible puncture needle (14-18 G) was placed subcutaneously outside the magnet.
The 38 biopsies were performed by eight radiologists with different levels of experience. The median procedure time was 103.5 minutes. Liver biopsies took significantly longer (mean = 134 minutes, ranging from 57 to 194 minutes) than soft-tissue biopsies (mean = 73.0 minutes, ranging from 30 to 121 minutes). In soft-tissue biopsies, the average preparation period was more than 43 minutes, and the preparation time was 63.5 minutes for liver biopsies.
"Optimization of the preparation period carries the highest potential to reduce the procedure duration," the authors stated. "Preinterventional planning imaging should not include diagnostic sequences, but should be restricted to the sequences which are strictly relevant for trajectory planning. Planning imaging should instead follow a short predefined standard protocol optimized for quick assessment."
In one liver biopsy, repositioning of the patient from a supine to a prone position was necessary, causing a total procedure duration of 161 minutes. This could have been avoided by better planning, they noted. Also, good communication between the interventional radiologist in the magnet room and the technician in the control room is essential. At the University of Tübingen, the in-room speakers and microphones must be turned off during image acquisition, so verbal communication during fluoroscopic sequences is not possible. A wireless MRI-compatible system that allows communication may lead to a more fluent procedure, they wrote.
This study has limitations, the authors admitted. The number of patients was relatively low, and since this was a retrospective study based on information in the PACS, only table times could be assessed, neglecting the time needed for positioning the patient on the table.



















