During the past three years, about 75 cardiac MR examinations per week have been performed at the London Chest Hospital, for a total of more than 7,000 exams. The current waiting time is six weeks, and to meet the rising demand, a new system will be installed by the end of 2011.
"Highly cooperative patients and slick teams reduce the time it takes to perform cardiac MR," consultant cardiologist Dr. Mark Westwood told delegates at the British Institute of Radiology (BIR) President's Conference in London. "Cardiac MR is fast, has reproducible results, and no ionizing radiation, and contrast is not required to look at ventricular function. You can take unlimited cardiac views, and if you have to, you can always do it again."
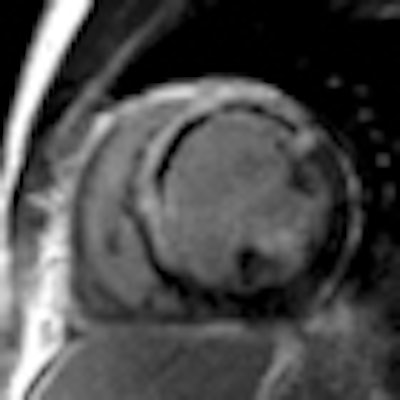
He uses the fast imaging employing steady state acquisition (FIESTA) sequence, which provides images of fluid-filled structures with very short acquisition times. It is vital that patients can tolerate lying flat for at least 20 to 30 minutes, and additionally patients must be able to hold their breath at certain points during the examination. Because of the breath-holds, the exam is often segmented for reading.
Retrospective gating involves synchronization of imaging with a phase of the cardiac cycle that allows capture of the whole cycle, but this only becomes an issue in cases of frequent ventricular ectopy. The images with well-controlled atrial fibrillation may be a little more blurred but nevertheless will be useful for diagnostic purposes, according to Westwood. Furthermore, MRI is very good for showing gross wall abnormalities, and for patients who are referred with chest pain for a stress perfusion scan for presumed coronary artery disease -- MRI may often discover hypertrophic cardiomyopathy.
 Late gadolinium enhancement image shows a large anteroseptal myocardial infarction (white arrow) with a central core of microvascular obstruction (red arrow). Images courtesy of Dr. Mark Westwood.
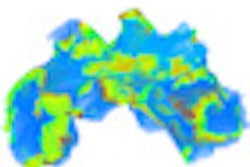
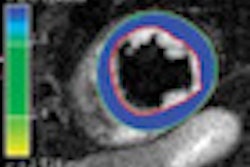
Late gadolinium enhancement image shows a large anteroseptal myocardial infarction (white arrow) with a central core of microvascular obstruction (red arrow). Images courtesy of Dr. Mark Westwood."Cardiac MRI provides reliable anatomical and functional assessment of the heart and evaluation of myocardial viability and coronary artery disease," he explained. "It is especially useful for diagnosing myocardial infarction. Cardiac MR late gadolinium enhancement can quantify the size, location, and transmural extent of the infarct."
A T1-weighted examination, using late gadolinium enhancement, should be produced to assess viability post-myocardial infarction. Because there is always a delayed washout with gadolinium in fibrotic myocardium, cardiac MR can identify those areas of delayed enhancement that correlate with the infarcted region.
"The biggest technical error doctors can make with late gadolinium enhancement technique is the potential for overdiagnosing dilated cardiomyopathy due to the appearance of darkened vessels as a result of flow effect, and loss of signal due to poor uptake of gadolinium in scarred myocardium," Westwood cautioned.
Diagnosis of viability is arrived at by pairing late gadolinium enhancement scans with functional images; the impairment of contractility, which is often seen on MRI, is referred to as hibernating myocardium.
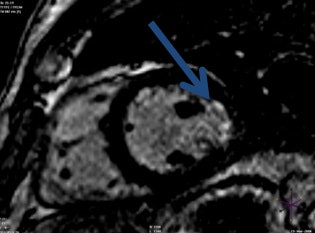 Late gadolinium enhancement image shows a small subendocardial lateral myocardial infarction (blue arrow).
Late gadolinium enhancement image shows a small subendocardial lateral myocardial infarction (blue arrow).For cardiac MR perfusion exams, the necessity to induce hyperemic stress in patients can be achieved by administering adenosine for four minutes (or dobutamine if adenosine is contraindicated) followed by rest. The difference between late gadolinium enhancement and perfusion exams is that radiologists watch whilst the gadolinium washes in, he said. Patients must avoid caffeine for six hours prior to the procedure. Because of the likelihood of patients requiring serial images over time during their disease process, it is essential to be consistent in procedural techniques, especially when performing perfusion exams; making a comparative analysis from previous scans to more recent ones can be made more difficult if varying techniques are used.