CT with a 320-detector-row scanner holds several advantages for CT angiography (CTA) of patients with atrial fibrillation and suspected coronary artery disease, concludes a study published online in European Radiology.
The ability to image patients with slower heart rates in a single beat, combined with high negative predictive value for all studies, ensures the 320-detector-row technique's clinical utility in a group of patients who have traditionally noninvasive imaging options. A proprietary algorithm designed to skip irregular heartbeats boosted image quality in the study, but at a cost of increased radiation dose, the authors said.
The challenge of atrial fibrillation
Multidetector-row coronary CTA does an excellent job of imaging most patients with suspected coronary artery disease, but atrial fibrillation has been a major challenge, wrote Lei Xu and colleagues from Beijing Anzhen Hospital in Beijing.
"Arrhythmia is considered a contraindication to [coronary CTA], because heart rate (HR) variation may lead to inappropriate data sampling and severe motion artifacts," they wrote (European Radiology, December 14, 2010).
However difficult it may be to scan patients with atrial fibrillation (AF), ruling out coronary artery disease (CAD) is important for patients with AF, the most common type of arrhythmia, whose incidence increases with age.
"AF is often associated with structural heart disease, but patients with AF may also have symptoms mimicking CAD," they wrote. "Therefore, the ability to discern the presence or absence of CAD is important in the treatment of patients with AF."
The quality of coronary CTA acquired with conventional MDCT has been inconsistent to poor. One study showed that the image quality of CTA decreased significantly when the heart rate exceeded 100 beats per minute (bpm), or when heart rate variability was greater than 24 bpm.
The 320-detector-row scanner has not been evaluated for use in patients with AF; hence, the study aimed to evaluate the feasibility, diagnostic accuracy, and radiation dose of coronary CTA in patients with atrial fibrillation.
The study included 37 patients (16 men, 21 women; mean age, 60.4 ± 6.3 years) with persistent AF and suspected coronary artery disease, who underwent both 320-detector-row coronary CT angiography and conventional coronary angiography.
Among the 37 patients, 27 were preparing for mitral valve surgery, nine for the treatment of AF, and one for surgical management of congenital heart disease. The patients had already been scheduled to undergo catheter-based coronary angiography for suspected coexisting CAD before the surgery.
All scans were performed using 320-detector-row CT (Aquilion One, Toshiba Medical Systems, Otawara, Japan) with 0.5-mm collimation. An arrhythmia rejection algorithm (version 4.51, Toshiba) was also used to skip beats that continuous electrocardiogram (ECG) monitoring indicated were irregular.
In patients with heart rates slower than 65 bpm, CT images were acquired in a single heartbeat. In patients with heart rates faster than 65 bpm, two to four heartbeats were used for data acquisition. Three heartbeats were used to acquire the imaging volume in patients with heart rates faster than 80 bpm, and four heartbeats were used in patients with heart rates faster than 110 bpm.
The CT data were evaluated for image quality and the presence of significant stenosis (≥ 50%) compared to catheter angiography. Two radiologists blinded to the results of conventional catheter angiography calculated the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of CT versus angiography as the reference standard.
High accuracy, NPV
The study evaluated a total of 474 segments 1.5 mm or larger based on the 17-segment American Heart Association model. Image quality was considered to be excellent in 162 (34.2%) patients, good in 247 (52.1%), moderate in 50 (10.5%), and poor in 15 (3.2%).
The 16-cm anatomic coverage of 320-detector-row CT enables the heart to be scanned in a single beat if the heart rate is 65 bpm or less, eliminating "stair-step" image artifacts that are inherent in 64-detector-row CT, which requires several gantry rotations to cover the volume of the heart, Xu and colleagues wrote.
Performance of 320-row CT patients with atrial fibrillation
|
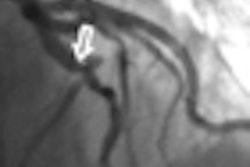
In all, three segments were overestimated and therefore false positive, including two segments with moderate calcification and one segment with motion artifacts.
Two segments were misdiagnosed as normal (false negative) due to low signal-to-noise ratio and small vessel diameter, including one segment with stenosis at the origin of the posterior descending artery and another segment in the distal left circumflex artery.
Although high heart rates did not degrade image quality significantly, heart rate variability rendered some studies nondiagnostic, the authors wrote. Tube current greatly affected the radiation dose.
"Reducing tube voltage from 120 to 100 kV was used when the patient's [body mass index (BMI)] was below 24 kg/m2 and the tube current was adjusted according to patients' thoracic anatomy and the size of the left atrium," Xu and colleagues reported. "Dramatic dose reduction was achieved with 100-kV protocol."
Estimated radiation dose variations by tube current and number of heartbeats
|
|||||||||||||||
| Radiation dose rose significantly when additional heartbeats were required for imaging. |
"In patients with AF and HR below 65 bpm, one-heartbeat acquisition in 320-detector-row [coronary CTA] is feasible, and avoids the misalignment of images caused by variation in RR intervals from the different heartbeats," they wrote. "This method makes coronary imaging accurate in AF patients with the reconstruction at around 70-75% of the RR interval without impairment of image quality."
Patients with faster hearts needed acquisitions lasting two to four heartbeats to enable the use of multisegment reconstruction and to improve temporal resolution, the group explained. Images reconstructed at end systole and absolute intervals for reconstructions are more suitable for patients with both atrial fibrillation and high heart rates, they added.
Motion artifacts "were the main cause of image quality degradation in our study, and high-quality images were obtained with reconstructions performed in the end-systolic phase in most patients with AF and higher HR," Xu and colleagues wrote.
In the 474 segments, image quality was considered as excellent in 162 segments (34.2%), good in 247 (52.1%), moderate in 50 (10.5%) and poor in 15 (3.2%). The segments with poor image quality included six right coronary artery segments, five left anterior descending segments, and four left circumflex segments.
No significant difference was found between 320-detector-row coronary CTA and conventional coronary angiography in the detection of significant stenosis (p = 1.000). The mean effective dose for coronary CTA was 13.0 ± 4.7 mSv.
320-detector-row CT depicted 96.8% diagnostic coronary segments, in line with previous studies. "The analysis of coronary artery stenosis shows promising results," the authors wrote. A limitation of 320-detector CT is insufficient temporal resolution, they added.
Generally the presence of calcifications, motion artifacts, and small vessel diameter impeded image interpretation, creating false-positive and false-negative results, they concluded.
"320-detector CT reliably provides diagnostic quality images of the coronary arteries in patients with AF," Xu and colleagues concluded. "The high negative predictive value makes 320-detector [coronary CTA] a potential replacement for invasive coronary angiography in the care of patients with AF and structural heart disease who need CAD ruled out before surgery."
By Eric Barnes
AuntMinnie.com staff writer
February 8, 2011