Computer-aided detection (CAD) technology can offer significant clinical value in diagnosing acute pulmonary embolism (PE), if a recent study presented at the 2010 European Congress of Radiology (ECR) in Vienna, Austria, is any indication.
A Dutch research team found that CAD positively impacted nearly one in four cases evaluated for PE in a year-long study. In addition, the use of CAD as a second reader yielded a statistically significant improvement in sensitivity for all six readers in the study, without affecting specificity.
These gains did come at the cost of long image interpretation times, however, said presenter Dr. Rianne Wittenberg of Academic Medical Center in Amsterdam, Netherlands.
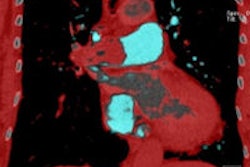
A potentially fatal disease, PE often has vague and nonspecific clinical symptoms, requiring medical imaging. In most institutions today, MDCT is the technique of choice for detecting PE, but it's time consuming and challenging to scroll through the 300 to 500 slices per CT scan while analyzing complex anatomic structures, she said.
To see if CAD can help decrease both radiologist workload and the chance of perception errors, the researchers evaluated the effects of a prototype CAD software (Philips Healthcare, Andover, MA) on observer performance for detecting acute PE. Six readers with varying levels of experience read CT pulmonary angiography (CTPA) studies from 215 consecutive patients referred to the radiology department for suspected PE between May 2007 and May 2008.
Of the 215 exams, 24% were positive for PE and 76% were negative. Six scans were excluded from the study due to technical failure of the CAD system.
For the purposes of the study, the reference standard was determined by independent reading of the exams by a trained researcher and an experienced radiologist. Any discordant findings were settled by another experienced chest radiologist.
The readers were asked to read the studies first without CAD and then with CAD as a second reader in one reading session. They documented the diagnosis, recorded the reading time, and gave a confidence score on a nine-point scale ranging from 1 (definitely no PE) to 9 (definite PE).
CAD led to a statistically significant increase in sensitivity (p = 0.014); the biggest improvement was seen with an inexperienced resident, climbing from 77% to 90%. However, a more experienced radiologist had the second biggest increase, climbing from 88% to 96%.
Ten patients in total benefited from the use of CAD, including four cases of segmental emboli and 11 subsegmental emboli, she said. CAD did not significantly improve the already relatively high specificity of the readers, which ranged from 89% to 98% without CAD, Wittenberg said.
"However, it also did not decrease the specificity, meaning that most of the false-positive CAD markings were easy to dismiss by the readers," she said.
False-positive CAD findings were attributed to reasons such as motion artifact and low arterial enhancement, she said.
Out of the 1,254 evaluations (six readers reading 209 cases), CAD was beneficial in 24%, according to Wittenberg. In 29 cases, CAD led to a correction of diagnosis; an increased confidence in the correct diagnosis was seen in 270 cases.
In 2% of cases, however, CAD had a detrimental effect. Eleven cases resulted in a change to an incorrect diagnosis, while 18 cases had a decrease in confidence in the correct diagnosis.
The number of inconclusive cases remained relatively constant, with 38 before CAD and 36 after CAD.
CAD extended reading time an average of 22%, but this differed significantly between readers (p < 0.001), she said. A significant correlation was also found between the number of false-positive findings per scan and additional reading time.
"At the expense of increased reading time, CAD has the potential to increase reader sensitivity and confidence for diagnosis of PE without loss of specificity," she said.
By Erik L. Ridley
AuntMinnie.com staff writer
March 26, 2010
Related Reading
MSK applications could give CAD a shot in the arm, February 12, 2010
Survey: CT most popular choice for suspected PE, December 23, 2009
CT supplants V/Q scanning for pulmonary embolism detection, October 20, 2009
CAD may improve novice performance in pulmonary CTA, March 26, 2009
Teleradiology can speed pulmonary CTA reads, March 23, 2009
Copyright © 2010 AuntMinnie.com