FDG-PET scans of non-small cell lung cancer (NSCLC) patients reviewed before radiation therapy (RT) may lead to significant changes in treatment strategy and radiation therapy planning, according to a study in the August issue of the American Journal of Roentgenology.
The French multicenter study found that the additional data provided by FDG-PET resulted in changes in planned RT strategy or in the detail of planned radiation therapy in 52 of 134 patients (39%). The lead author of the study was Pascal Pommier, MD, from the department of radiation oncology at Lyon University-Centre Léon Bérard in Lyon, France (AJR, August 2010, Vol. 195:2, pp. 350-355).
Clinical decisions
The objective of the study was to determine how pre-radiation-therapy FDG-PET scans would affect a physician's decision for curative or palliative treatment for a patient with non-small cell lung cancer.
Between January 2004 and July 2006, researchers enrolled 148 patients from the 11 participating medical centers. The patients were younger than 76 years of age with inoperable stage I, II, IIIA, or IIIB NSCLC and were scheduled for 3D conformal radiation therapy. Fourteen of these patients were later excluded from the study for not complying with protocol criteria.
Of the remaining 134 patients, 48 (36%) had a history of past or current respiratory disease with moderate to severe chronic respiratory insufficiency, and 105 (79%) were diagnosed with stage III disease.
Chemotherapy had been administered to 110 patients (82%). For 25 of those patients, the prechemotherapy workup included FDG-PET. The FDG-PET findings were available when the initial decision on radiation therapy strategy was made.
Planned treatment
Conventional CT and FDG-PET scans were performed two to three weeks before the scheduled start of radiation therapy. Physicians were asked to plan radiation therapy for the patients without benefit of the FDG-PET images. When FDG-PET results were available, physicians were asked to confirm their radiation therapy strategy and to determine whether any treatment changes were necessary.
FDG-PET scans of the 134 patients were acquired in rotating projections and in axial, coronal, and sagittal planes. Nuclear medicine physicians analyzed the images after intravenous administration of 3 to 6 MBq/kg of FDG and visually evaluated the results as positive or negative.
Standardized uptake values (SUVs) were compared with SUVs in the liver; lesions with SUVs greater than those of the liver were classified as malignant.
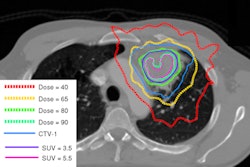
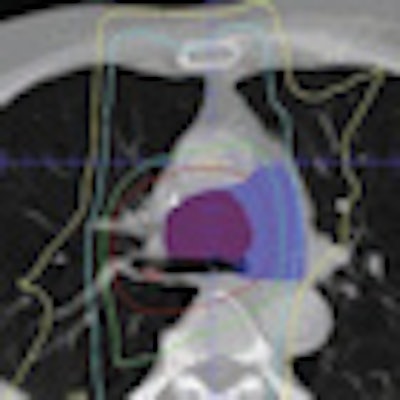
In addition, Pommier and his colleagues calculated a clinical target volume (CTV), which included the pre-radiation-therapy tumor volume based on an initial contrast-enhanced CT and postchemotherapy contrast-enhanced CT. The clinical target volume took into account the tumor reduction after chemotherapy in lateral, anterior, and posterior directions. Nodes with a short axis more than 10 mm in diameter were considered positive and were included in the target area. All areas of FDG uptake considered malignant also were included in the volume.
FDG-PET's influence
After review of the pre-radiation-therapy FDG-PET images, the researchers canceled planned curative radiation therapy for 15 patients. FDG-PET showed the need for the clinical target volume to be enlarged for eight patients, while the treatment strategy for six patients changed due to the discovery of metastases. FDG-PET also helped determine the need for surgery, rather than radiation therapy, for one patient.
Subsequently, palliative chemotherapy was performed on eight patients and palliative radiation therapy on six patients.
FDG-PET also confirmed an indication for curative radiation therapy in 119 patients (89%), with pre-radiation-therapy FDG-PET modifying the initial RT plan in 37 (31%) of the 119 patients. "The concordance rate between the treatment strategies with or without pre-radiation-therapy FDG-PET was 62%," the authors added. "Concordance was improved but was still not complete (80%) when the prechemotherapy workup included FDG-PET."
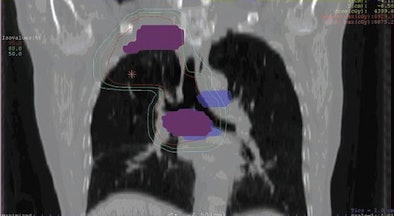 |
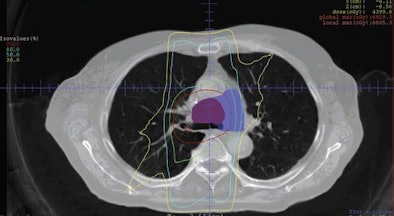
| Images are of a 62-year-old man with NSCLC. Initial pre-FDG-PET and clinical target volume (CTV) are represented in blue and red, respectively, on frontal (above) and transverse (below) images. FDG-PET images resulted in a decrease of mediastinal CTV and treated volume. Isodose lines represent dose distribution (95%, 80%, 50%, and 30% of prescribed dose). Images courtesy of the American Journal of Roentgenology. |
 |
Major modifications, defined as a change of more than 10% of the prescribed dose or more than 25% of the clinical target volume, occurred in 21 patients (18%), with the total prescribed radiation therapy dose modified in 13 patients (10%), and modified by more than 10% of the initial prescribed dose in three patients.
Pre-radiation-therapy FDG-PET data induced a modification of the clinical target volume in 33 patients (25%), and 19 patients (14%) had a modification of more than 25%.
Nine patients had both their clinical target volume and radiation dose altered, with a greater target volume prompting a decrease in total radiation therapy dose in six patients. Conversely, a reduction of the target volume resulted in a greater radiation therapy dose in five patients.
'Major implications'
The results show "major implications for practice of pre-radiation-therapy FDG-PET, thus supporting the use of pre-radiation-therapy FDG-PET when deciding on treatment strategy and planning radiation therapy in non-small cell lung cancer, even if FDG-PET has been performed at the initial workup," Pommier and colleagues concluded. "A prospective evaluation of patient outcome (including sites of recurrence and toxicity) is warranted to assess the clinical relevance of this strategy."
The authors noted that their study did not consider long-term outcome and did not include data on the site of recurrence or overall survival. "Therefore," they added, "whether the resulting modifications in the treatment plan will significantly improve tumor control and quality of life has still to be shown."
By Wayne Forrest
AuntMinnie.com staff writer
August 11 2010
Related Reading
PET/CT beats CT in NSCLC staging, but both have limitations, July 2, 2010
ASTRO: Use PET for NSCLC judiciously, November 3, 2009
FDG-PET/CT aids in radiation therapy planning, March 5, 2008
PET does not predict survival in advanced lung cancer, November 29, 2007
PET/CT planning allows for greater gamble on NSCLC radiotherapy, March 16, 2005
Copyright © 2010 AuntMinnie.com