Two studies recently published online in Radiology yield important new information about CT-detected part-solid lung nodules. Mass measurements of ground-glass nodules are the most accurate, say Dutch researchers, but a Korean group found that most part-solid nodules not only disappear over time -- they do so in predictable ways.
First, researchers from the Netherlands reported that mass measurements of ground-glass nodules are far less variable than other methods and also are better predictors of malignancy. In a second study, Dr. Sang Min Lee and his team from Seoul, South Korea, found that most part-solid nodules were transient and predictable based on imaging and patient factors. Together, the studies yield important implications for managing nodules detected at CT lung cancer screening.
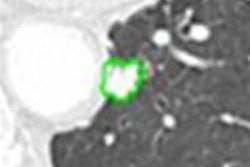
In a study published online February 1, 2010, Dr. Bartjan de Hoop from University Medical Center in Utrecht, Netherlands, and colleagues described the broad range of benign conditions, such as fibrosis or inflammatory disease, that can be depicted as ground-glass nodules (GGN) at CT. But there is scant assurance in those findings; the group noted that most malignancies detected in the Early Lung Cancer Action Program (ELCAP) studies have been diagnosed from GGN.
Because early growth is a critical indicator of malignant risk, it makes sense to perform volumetric assessments of screening-detected nodules. However, mass measurements aren't yet routine for GGNs.
"Nodule volumetry is superior to diameter measurements in solid nodules in terms of accuracy and reproducibility, but volumetric measurement techniques are not yet used regularly for GGNs," wrote de Hoop and co-authors including Dr. Hester Gietema, Ph.D., Saskia van de Vorst, and Dr. Mathias Prokop, Ph.D. "Mass is a parameter that integrates volume and density: Mass increases if the volume of a nodule increases, or if its density increases. Mass shouldn't therefore be suitable for identifying GGNs with a high risk for malignancy."
The study compared manual measurements of diameter, volume, and mass of pulmonary GGNs to determine which method is best for identifying malignant nodules by measuring change over time. The scans were acquired at 16-detector-row CT (MX800 IDT or Brilliance 16, Philips Healthcare, Andover, MA) at 16 x 0.75-mm collimation, 30 mAs, and 120-140 kVp.
The researchers performed baseline and follow-up measurements of 52 GGNs, with two investigators measuring the nodules with electronic calipers, manually outlining them to obtain volume and mass, and scoring for the presence of solid components. One of two expert observers repeated all of the measurements two months later. Bland-Altman analysis was used to calculate coefficients of variation and limits. Interobserver variability between measurement methods was also assessed.
From a total of 2,994 volunteers who were scanned, 52 GGNs were detected in 45 participants (42 men, 3 women; mean age, 62 years; range, 53-73 years). The median nodule diameter was 13.9 mm (range, 3.9-29.7 mm)
One benign and 13 malignant GGNs were resected in 12 patients (two of the patients each had two malignancies), with a median diameter of 18.2 mm (range, 8.6-29 mm), including adenocarcinoma (n = 7), bronchoalveolar carcinoma (n = 6), and atypical adenomatous hyperplasia (n = 1).
According to the results in all GGN, the κ values for intra- and interobserver agreement for identifying a solid component were 0.55 and 0.38, respectively. Both intra- and interobserver coefficients of variation were smallest for mass measurement of GGN (p < 0.001), with mean growth-to-variability ratios of 11, 28, and 35 for diameter, volume, and mass methods, respectively (p = 0.03).
Calling their study the first mass-based analysis of changes in GGNs, the results show that "for the evaluation of potentially malignant GGNs, measurement of GGN mass has lower inter- and intraobserver [variability] than do manual volume and diameter measurements," they wrote. "The lower variability [of mass measurements] resulted in a significantly improved ability to detect growth. ... This observation was confirmed by a significantly shorter time required for change in mass to exceed measurement variability compared with the time required for diameter and volume measurements."
Because GGNs grow so slowly, the increased ability to detect such changes can be critical for finding lesions at highest risk of malignancy in time for curative resection. And because mass measurements give greater weight to attenuation, they can find risky growth patterns not visualized in other methods. Development of a solid component is often used to differentiate benign from malignant findings.
"The development or progression of a solid component within a GGN influences GGN mass, but it does not directly influence GGN diameter or volume," they noted. "As a result, the growth-to-variability ratio was greater for mass than for volume or diameter, which makes mass measurement superior to the other techniques for detecting growth."
Transient ground-glass nodules are predictable
While it's known that many ground-glass nodules at CT represent nonmalignant etiologies and therefore disappear over time, the Korean study aimed to determine if the transience of part-solid nodules followed predictable patterns.
Because the malignancy rate of ground-glass nodules has been reported to be higher than that of solid nodules, the New York Early Lung Cancer Action Program regards part-solid nodules (PSNs) 5 mm and larger as positive findings with recommended further workup. But they are not often persistent; a recent report found that approximately 49% of solitary part-solid nodules detected at baseline CT were transient.
This finding suggests that lesion size may be a poor indicator of the need for workup, lest patients be subjected to "unnecessary radiation exposure, invasive procedures, and unnecessary financial burden, as well as psychiatric stress during further workup," wrote Dr. Sang Min Lee and colleagues from Seoul National University College of Medicine (Radiology, published online February 19, 2010).
Their study sought to evaluate such lesions retrospectively, in an effort to assess features that might predict which ground-glass opacities would be transient or persistent, to better determine the best patient care strategy.
Among 6,777 individuals who underwent chest CT between 2006 and 2008, the researchers detected 126 part-solid nodules in 93 individuals from the hospital's database.
Then the team reviewed the clinical features and CT characteristics, comparing clinical and thin-section CT features between transient and persistent part-solid nodules. The group performed logistic regression analysis and statistical analysis to identify predictive factors of transient part-solid nodules.
All 93 subjects had at least two noncontrast thin-section exams (mean, 2.82 exams), with a mean CT follow-up period of 331.1 days (range, 34-965 days). Most exams (176 of 183) were acquired on a 16-detector-row scanner, with the remaining exams performed on eight- (n = 3) and 64-detector-row CT (n = 4).
Images were acquired using 1.0 to 1.25-mm collimation and reconstruction, 120 kVp, 40-mAs, and a medium-sharp reconstruction algorithm (B50F). Two experienced readers blinded to the results evaluated all images for size, location, margins and borders, size of the solid portion of the nodule, bubble lucency, air bronchogram, and pleural retraction. Shape was not assessed, but the average measure of height and width was used to determine lesion size.
In all, they found that 69.8% (88 of 126) of the part-solid nodules were transient (mean diameter, 11.3 mm; significantly larger than persistent nodules). Also significant (p ≤ 0.05) were differences between transient and persistent part-solid nodules in patient age, gender, risk of lung cancer, presence of eosinophilia, mode of detection, lesion size, lesion multiplicity, size of solid portion, and lesion border.
Multivariate analysis showed that young patient age, lesion detection at follow-up, having multiple lesions, blood eosinophilia, large solid component, and poorly defined lesion borders were all significant (p ≤ 0.05) independent predictors of transient PSNs, the authors wrote. Moreover, using a logistic regression model that incorporated clinical as well as imaging features substantially improved the ability to predict a transient lesion.
In line with previous studies, transient lesions were found more frequently in younger patients, male patients, and current smokers, the group noted.
"It has been shown that smoking could be a cause of respiratory bronchiolitis, desquamative interstitial pneumonitis, or inflammatory lesions and that these diseases can manifest as [ground-glass opacities] and are likely to be transient," the researchers wrote. "In addition, considering that pulmonary eosinophilia was more frequently shown in men and current smokers, the relationship between transient PSNs and smoking and male sex could be linked to the high proportion of blood eosinophilia in individuals with transient PSNs."
Lesions in all 15 current smokers in the study were transient, underscoring the authors' suggestion that smoking may cause transient and inflammatory lesions far more frequently than persistent part-solid nodules, though further study is necessary, the authors added.
They also noted that blood eosinophilia is another common cause of transient inflammation in the lung, common in current smokers.
"Spiculated margin, air bronchogram, and pleural retraction could also be very useful in differentiating persistent from transient PSNs because none of the transient PSNs in our study showed those CT findings, although we did not include them in the logistic regression analysis because of statistical reasons," they wrote.
Using both clinical and thin-section CT features, "transient PSNs could be predicted with high accuracy," the group concluded.
By Eric Barnes
AuntMInnie.com staff writer
February 24, 2010
Related Reading
Lung CAD boosts radiologist accuracy, February 17, 2010
New TNM scale accurate for predicting lung cancer survival, January 11, 2010
CT lung CAD helps readers differently, November 4, 2009
CARS report: New CAD tool follows lung nodules over time, June 30, 2009
Management strategies evolve as CT finds more lung nodules, August 19, 2005
Copyright © 2010 AuntMinnie.com