In a new study from Poland, perfusion CT showed impressive accuracy for distinguishing benign from malignant lymph nodes in a study of squamous cell cancer patients with suspected metastases.
Researchers said they got little help from routine contrast-enhanced CT in their study of 138 nonenlarged nodes in 63 patients. On the other hand, histopathology confirmed the high accuracy of perfusion CT findings in nearly all cases -- proving its potential to improve the management of patients with head and neck cancers.
"Malignant lymph nodes have deformed vascular structure and different hemodynamics due to the distortion of normal nodal architecture and neovascularization. Therefore, malignant nodes should have perfusion alterations," said Dr. Agneistsa Trojanowska from the Medical University of Lublin in Lublin, Poland.
When the group began its work in 2006 there were no published CT perfusion studies on the topic, Trojanowska said in a talk at the 2009 RSNA meeting. Beginning with their first 12 patients in 2007, however, the researchers have examined a total of 63 patients with suspected malignant metastases.
"All patients suffer from either otolaryngeal cancer [n = 38] or oral cavity cancers [n=25], Trojanowska said. "They were proven by biopsy to be squamous cell cancers. All patients were previously untreated and they were considered surgical candidates."
The group used CT perfusion in an effort to determine which parameters could be used to differentiate nonenlarged malignant from nonmalignant cervical lymph nodes.
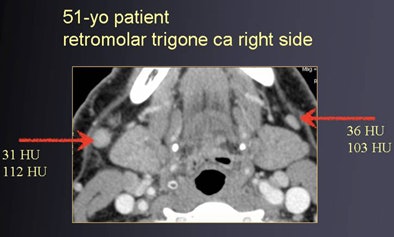 |
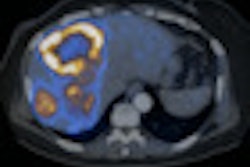
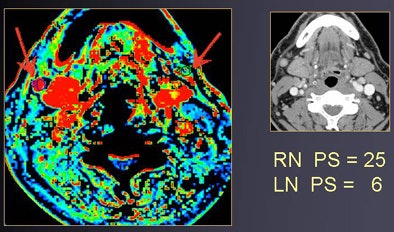
| Round shape (contrast-enhanced CT, above) suggests suspect nodes in a patient with right-sided oral cancer. At perfusion CT (below), relative blood volume and permeability surface area product values of right lymph node are elevated compared to the contralateral side, showing hyperperfusion. Histopathology confirmed the malignancy. All images courtesy of Dr. Agneistsa Trojanowska. |
 |
All images were acquired on a 64-detector-row scanner (LightSpeed VCT, GE Healthcare, Chalfont St. Giles, U.K.) a mean 11 days before surgery at 1.25-mm collimation. CT perfusion images were acquired immediately after contrast-enhanced CT scans (80-100 mL iodinated contrast at 1 mL/sec injected after a 100-sec scan delay).
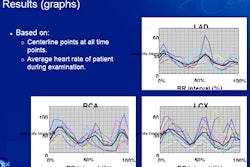
Perfusion maps were created automatically (CT Perfusion 4, GE Healthcare) for relative blood volume (rBV), relative blood flow (rBF), mean transit time (MTT), and permeability surface area product (PS) for every node with a short axis of 5 mm or longer, Trojanowska said.
Perfusion values were then evaluated using manually modified regions of interest (ROIs) for each node separately, based on the average results of two experienced readers for each node. Unilateral or bilateral biopsy was performed in all patients to check the results. Suspect nodes were resected separately and their positions marked on axial, sagittal, and coronal reformations and discussed with the surgeon. Specimens underwent fixation, H&E staining, and standard histopathologic analysis.
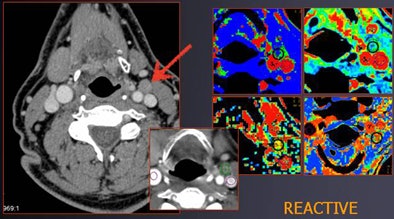 |
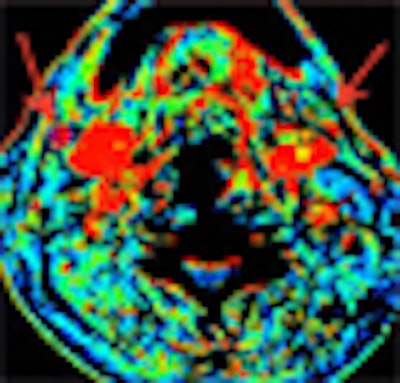
| A patient with tongue cancer had a known right-sided malignancy and a suspect node at left side. Normal rBV (2.7) and rBF (55) values suggest a reactive condition; histologic analysis confirmed the benignity of the node (MTT = 6.2, PS = 14). |
The researchers then correlated CT perfusion results with histology for all nodes 5 mm and larger that were:
- Small (but not < 5 mm short axis)
- Without central necrosis
- Upper cervical nodes due to primary tumor site (at cervical bifurcation and above)
- Near tumors
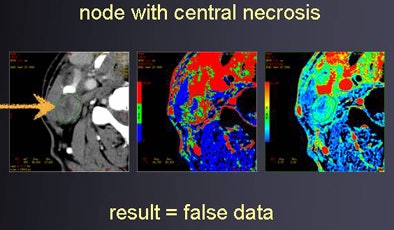
At least one node was included from the contralateral side in each patient, and from groups most suspected for metastasis, Trojanowska said. "We excluded nodes with central necroses -- after a few cases, we realized that in nodes with central necrosis, perfusion values were very low," she said.
In all, 190 nodes were removed in 63 patients; of these, 138 were matched with histology, revealing 82 malignant and 56 nonmalignant nodes. All perfusion studies were interpretable.
"It was clear that blood flow blood volumes were much higher for metastatic compared to benign nodes; also, the permeability surface area product was almost as twice as high compared to benign lymph nodes," Trojanowska said. "So the conclusion from these is that metastatic lymph nodes are characterized by hyperperfusion."
|
CT perfusion's sensitivity, specificity, and accuracy for the characterization of lymph node malignancy were 97%, 79%, and 87%, respectively, she said.
"The CT perfusion exam provides additional information regarding the characterization of lymph nodes, and it might be useful in further studies for differentiation of malignant and normal nodes," she said.
An audience member asked Trojanowska whether it might be possible to include necrotic lymph nodes by simply selecting an alternative ROI that excludes the necrotic region.
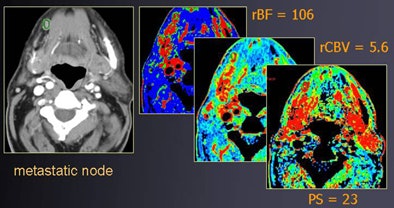 |
| Patient with oral cancer shows very high values for rBF, rBV, and PS; lymph node was found to be malignant at histology. |
"Necrosis could affect the perfusion values, and we should not use a different ROI," Trojanowska responded. "First, we did not evaluate nodes with necrosis because the necrosis itself is the most significant factor that proves the malignant character of the lymph node; so, in our opinion, it was useless to evaluate lymph nodes with central necrosis because it's almost sure that it's malignant."
Second, she said, if one opts to avoid the necrotic ROI by zeroing in on peripheral tissue for the perfusion analysis, "it's very probable that this tissue will be very hypoperfused for several reasons -- and you might make a mistake" in diagnosis.
 |
A session moderator questioned the value of perfusion CT in the presence of a micrometastasis, which might not demonstrate enhanced perfusion.
By Eric Barnes
AuntMinnie.com staff writer
January 25, 2010
Related Reading
FDG-PET/CT trumps CT in detecting anal carcinoma, November 25, 2009
PET/CT directs head and neck cancer treatment, November 17, 2009
FDG-PET/CT scans spot head and neck cancer return, October 14, 2009
Axillary ultrasound can help avoid sentinel node biopsy surgery, October 8, 2009
Copyright © 2010 AuntMinnie.com