Virtual colonoscopy (VC or CT colonography [CTC]) is generally accepted as an effective and reliable screening tool for polyps and cancer. But laxative-based bowel-cleansing methods can be uncomfortable and inconvenient for patients.
To improve the patient experience, recent studies have sought to eliminate cathartic cleansing and rely instead on fecal tagging using iodinated oral contrast agents, which have a mild cathartic effect of their own.
At present, no fecal-tagging preparation has gained widespread acceptance in the virtual colonoscopy community. However, as reported recently at the 2008 European Congress of Radiology (ECR) in Vienna, several new studies have evaluated different preparations in an attempt to achieve a good compromise between image quality and patient tolerance.
In a study that compared two different doses of an iodinated VC fecal-tagging agent, Dr. Marjolein Liedenbaum and a group of researchers from the Academic Medical Center in Amsterdam, Netherlands, found the lower dose preferable to the higher one. Greater sensitivity and specificity were also achieved, though not significantly, using 75% less of an iodinated oral contrast agent, while patient acceptance was significantly improved.
The study examined 99 patients with a positive a fecal occult blood test, who were split into two groups before undergoing CT colonography. One group was given 7 x 50 mL of Telebrix Gastro (meglumine ioxithalamate, 300 mg of iodine/L), while the other received just 4 x 50 mL, all combined with a low-fiber diet. The researchers did not use a traditional cathartic cleansing method, preferring to prepare the bowel with the iodine tagging agent alone. The results were compared through colonoscopy with segmental unblinding.

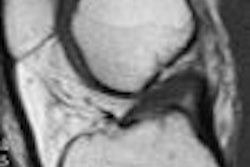
| A colon lumen filled with tagged feces -- a typical image with Telebrix preparation. Image courtesy of Dr. Marjolein Liedenbaum. |
"The contrast agent still gave some diarrhea, but the burden from this CTC bowel preparation was less than the extensive cathartic preparation these patients received at their colonoscopy," noted Liedenbaum.
Residual stool attenuation and homogeneity were measured per colonic segment, while two reviewers performed lesion (polyp and carcinoma) detection. A questionnaire developed at the institution was used to assess patient acceptance of each protocol.
The results showed that tagging density was 637 HU for the 7 x 5-mL group and 615 HU for the 4 x 5-mL group, while homogeneity (standard deviation of attenuation) was 92 HU and 86 HU, respectively. The differences in the amount of residual stool and tagging quality were not significant.
In identifying lesions at least 10 mm in size, sensitivity per patient in the higher-dose group was 90%, compared with 96% in the lower-dose group. Specificity per patient (identifying patients without lesions of 10 mm or greater) was 100% for both reviewers in the lower-dose group, compared with an average of 96.5% for the higher-dose group.
Patient acceptability regarding the burden of diarrhea was also significantly improved for those in the lower-dose group, leading Liedenbaum's group to conclude that in this case a higher dose of contrast agent yields no benefits in VC but can lead to a worse patient experience and poorer compliance.
"Image quality was certainly not worse in the lower-dose group, and patient acceptance was better," Liedenbaum told AuntMinnie.com. "I would advise the use of this lower dose."
Three regimens in Italy
In related work, researchers in Italy saw some interesting outcomes when comparing three different fecal-tagging VC preparations in a 180-patient study. Three groups of 60 patients underwent virtual colonoscopy on a 16-slice scanner after following a low-residue diet and adhering to one of three regimens:
- Group A: Three sachets of Movicol (dipolyethylene glycol, Norgine, Harefield, U.K.) two days before VC, plus 50 mL of Gastrografin (Bracco, Milan) in 1 liter of water two hours before examination
- Group B: 2 mL/kg of Gastrografin two days before VC
- Group C: 90 mL of Phospho-soda (Fleet Pharmaceuticals, Lynchburg, VA) plus 100 mL of Gastrografin one day before VC
The objective was to compare different laxative preparations and the consequences of changing the administration timing, which can have notable effects on a patient's comfort and compliance with the procedure. Before undergoing VC, patients expressed their tolerance to the preparation according to a 10-point scale (0 = no discomfort, 10 = high discomfort).
Results indicated that same-day preparation (group A) was tolerated significantly better than group C (p < 0.05), whereas no statistically significant differences were observed when comparing the other groups.
"It is also worth noting that most patients who underwent the same-day preparation indicated minor to no discomfort at all. In fact, 75% of the patients ranked their discomfort as 2 or lower on the 10-point scale," said Dr. Delia Campanella of the Institute for Cancer Research and Treatment in Turin, Italy.
"In our opinion, this is due to the absence of a strong laxative in group A -- Movicol has a minor laxative effect, but is really rather a stool softener than a true laxative. It also causes fewer side effects than sodium phosphate, which is used in the group C preparation," she explained.
"Finally, the total iodine intake is greater for group B (37 g maximum) and group C (55.5 g) than group A (18.5g). The higher dose increases the Gastrografin laxative effects and, thus, patient discomfort through side effects such as nausea and vomiting," she said.
 |
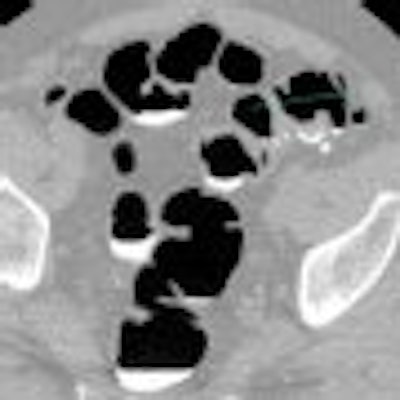
| CT colonography from group A (same-day preparation). The coronal image shows good and homogeneous fecal tagging from the proximal to the distal colon. Image courtesy of Dr. Delia Campanella. |
The relative performances of the three preparations, in terms of the quality of fecal tagging, was assessed by using commercially available computer-aided detection (CAD) software (iM3D, Turin, Italy). The key idea is that its performance depends on the quality of the preparation.
Results showed that CAD specificity was higher for group C compared with group A (p = 0.020) and group B (p = 0.001). Yet, to achieve this benefit, patients in group C were compromised most of all in terms of discomfort.
Overall, taking all factors into account, Campanella and her colleagues Drs. Lia Morra and Silvia Delsanto from iM3D found that the group A regimen could be considered the best preparation, particularly as there are myriad benefits to same-day administration and examination.
"Same-day preparation requires less contrast material (lower cost), is safer (administered on a hospital ward), is well-tolerated (no catharsis and therefore fewer side effects) and yields good-quality images, even if they are slightly inferior to those of group C," she concluded.
By Rob Skelding
AuntMinnie.com contributing writer
April 16, 2008
CT colonography effective with limited bowel preparation, April 10, 2008
Need for bowel prep prior to elective colorectal resection questioned, December 24, 2007
Noncathartic bowel prep facilitates, complicates virtual colonoscopy, June 15, 2007
Prepless VC yields high sensitivity in average-risk subjects, June 10, 2007
New developments improve VC -- and colonoscopy, April 6, 2007
Copyright © 2008 AuntMinnie.com