Patients with positive screening results on fecal occult blood tests (FOBTs) should probably head straight to optical colonoscopy for their next exam, according to a new study from the Netherlands. Virtual colonoscopy (also known as CT colonography or CTC) may not be cost-effective in this population because so many FOBT-positive patients would need referral for polypectomy anyway, the researchers said.
Dr. Marjolein Liedenbaum and colleagues from the Academic Medical Center in Amsterdam aimed to determine whether VC is clinically and economically effective for the triage of individuals with positive fecal occult blood test results. Liedenbaum presented the final results of the study, including a procedure cost analysis, at the 2009 European Congress of Radiology (ECR) in Vienna.
The fecal occult blood test is a cheap and simple test to detect colorectal carcinoma in screening populations, and previous studies have shown that it can reduce mortality from colorectal carcinoma by 60%, she said.
"But FOBT has its disadvantages," Liedenbaum said. "It generates a lot of false positives -- about 55% of patients who have a positive FOBT don't have any polyps or carcinoma at colonoscopy. So if we could use CTC as a triage technique in those FOBT positives, we could reduce the number of unnecessary colonoscopies."
The study, performed in three different institutions in Holland, screened almost 30,000 individuals with one of two commonly used FOBT tests; 302 participants (mean age, 61 years; male/female ratio, 1:1.6) were positive. Those with positive results were scheduled for colonoscopy, and, for the study, also underwent virtual colonoscopy.
The study considered a strategy of sending FOBT positives for triage with VC, versus sending them directly to optical colonoscopy. "We also considered the polyp and carcinoma resection and the costs," Liedenbaum said.
All patients scheduled for CTC received a noncathartic bowel preparation for one or two days consisting of an iodinated oral tagging solution (7 mL Telebrix, Guerbet, Roissy, France) combined with a low-fiber diet.
CTC was performed following automated CO2 insufflation (ProtoCO2l, Bracco Diagnostics, Princeton, NJ) with low-dose supine and prone scanning on a 64-detector-row scanner.
The consecutive screening participants who tested positive with guaiac (G-FOBT) or immunochemical (I-FOBT) tests (OC-Sensor, Eiken Chemical, Tokyo) then underwent CTC with an iodine tagging bowel preparation.
Two experienced readers working independently read each scan, calculating per-patient positive and negative predictive values (PPV and NPV) based on the double reading. All participants subsequently underwent conventional colonoscopy, and the CTC results were compared with segmentally unblinded colonoscopy results.
Data were analyzed in two categories based on polyp size: 10 mm and larger and 6 mm and larger. Sensitivity, specificity, and positive and negative predictive values were calculated using a 10-mm polyp cutoff size, Liedenbaum said.
"We calculated the cost of initial clinical management for the two strategies. The first strategy is CT colonography in all FOBT positives, and only in the CT colonography positives," Liedenbaum said. "The second strategy is to do colonoscopy in all FOBT positives, with no triage with CT colonography."
The group also evaluated patients' reactions by questionnaire after the exams. The survey results showed that participants considered colonoscopy to be significantly more burdensome than CTC, Liedenbaum said.
Of 302 FOBT positives included in the study (54 g-FOBT and 248 I-FOBT), 22 (7%) had a colorectal carcinoma, 142 (47%) had a lesion 10 mm or larger, and 210 (70%) had a lesion 6 mm or larger.
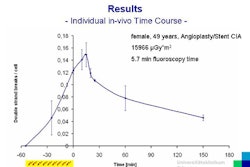
CTC results for FOBT-positive study participants by polyp size
|
||||||||||||||||||
"The unit cost of CTC in Holland was 179 euros [$240]," Liedenbaum said. "If we use a 10-mm size cutoff for the strategy of CTC first ... the cost was 322 euros [$431] per screened person. For direct colonoscopy [without CTC triage], the cost was 275 euros [$368] per screened person. This means that using CTC as a triage technique would generate additional costs of 17%."
Not included in the analysis were the costs of working up extracolonic findings, which apply only to VC and can result in additional expense (approximately $30 to $40 per exam in previous studies). The search for extracolonic findings can result in the discovery of clinically important abnormalities that save lives, on one hand, but it can also result in potentially unnecessary costs, procedures, and risks to the patient, on the other.
"We found that CT colonography with a limited bowel preparation is unlikely to be an efficient triage technique in first-round FOBT population screening," she concluded. "This is mainly due to the high true-positive rate in the FOBT-positive population, resulting in a high cost for triage."
By Eric Barnes
AuntMinnie.com staff writer
May 9, 2009
Related Reading
Fecal occult blood screening may help reduce colorectal cancer mortality, April 6, 2009
Screening CT colonography and colonoscopy similarly effective, February 18, 2009
Virtual colonoscopy beginners do better with 3D data, February 5, 2009
FOBT-screened cohort yields too many positives for VC, July 28, 2008
FOBT screening reduces emergency colorectal cancer admissions, March 25, 2008
Copyright © 2009 AuntMinnie.com