How does MRI compare with chest x-ray in detecting cardiac and noncardiac findings? Very similarly, according to new research from Italy. Both modalities identified pulmonary nodules, had similar pulmonary nodule detection rates, and more.
Nearly 300 consecutive patients underwent both MRI and chest x-ray less than seven days apart. The research team, led by Marco Alì, a doctoral fellow in integrative biomedical research in the radiology unit at the IRCCS Policlinico San Donato in Milan, found the two techniques performed comparably. Alì and his colleagues presented their findings in an e-poster at the 2018 European Society of Thoracic Imaging (ESTI) and European Society of Cardiovascular Radiology (ESCR) annual meeting in Geneva.
 A 73-year-old woman with a visible pulmonary nodule at MRI (left) and chest x-ray (right). All images courtesy of Marco Alì.
A 73-year-old woman with a visible pulmonary nodule at MRI (left) and chest x-ray (right). All images courtesy of Marco Alì.MRI vs. chest x-ray
Often, clinicians turn to chest x-ray for diagnosing pulmonary nodules. But what about using MRI? It has a superior ability to image soft tissue and the added bonus of no ionizing radiation. Can MRI be used instead? First things first -- the two techniques must be compared, which is exactly what Alì and colleagues did.
Between April 2014 and May 2016, a total of 287 consecutive patients underwent half-Fourier acquisition single-shot turbo spin-echo (HASTE) MRI and chest x-ray for cardiac and noncardiac findings. The researchers considered pulmonary nodules and infiltrates, pleural effusion, and cardiac and aortic enlargement. Two independent, blinded radiologists read the reports.
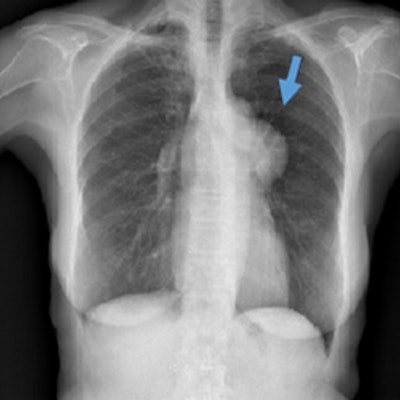
 A 32-year-old man with pleural effusion visible at MRI (arrow in panel a) but not clearly visible at chest x-ray (panel b).
A 32-year-old man with pleural effusion visible at MRI (arrow in panel a) but not clearly visible at chest x-ray (panel b).Both techniques had the same detection rate for pulmonary nodule detection: 1.7%. Interreader agreement was perfect for HASTE MRI and modest for chest x-ray. The pleural effusion detection rate for HASTE MRI was higher than chest x-ray, but their agreement was almost perfect. The pulmonary infiltrate detection rate at HASTE MRI was equivalent to that at chest x-ray, with an almost perfect intertechnique agreement. The interreader agreement was moderate for both HASTE MRI and chest x-ray. Results are summarized in the table below.
| Comparison of chest x-ray & HASTE MRI in Italy | ||
| Chest x-ray | HASTE MRI | |
| Pulmonary nodule detection rate | 1.7% (5/287) | 1.7% (5/287) |
| Pulmonary nodule detection interreader agreement | κ = 0.393 | κ = 1.0 |
| Pleural effusion detection | 13.9% (40/287) | 19.1% (55/287) |
| Pleural effusion detection interreader agreement | κ = 0.773 | κ = 0.902 |
| Pulmonary infiltrate detection rate | 7.7% (22/287) | 8.4% (24/287) |
| Pulmonary infiltrate interreader agreement | κ = 0.554 | κ = 0.639 |
In terms of cardiac enlargement, the detection rate of HASTE MRI (45.3%, 130/287) was borderline significantly lower (p = 0.057) than that of chest x-ray (48.1%, 138/287). The two had an almost perfect intertechnique agreement (κ = 0.902). The interreader agreement was substantial for both HASTE MRI (κ = 0.798) and chest x-ray (κ = 0.744).
Regarding aortic dilation, the detection rate at HASTE MRI (17.7%, 51/287) was significantly higher (p < 0.001) than that at chest x-ray (9.7%, 28/287), with a substantial intertechnique agreement (κ = 0.648). The interreader agreement was moderate for both HASTE MRI (κ = 0.724) and chest x-ray (κ = 0.346).
Alì and colleagues plan to continue their line of research.
"After evaluating our results, we found a gap in the literature concerning the comparison between HASTE MRI and CT as a reference standard," he told AuntMinnieEurope.com. "We would also like to conduct prospective intraindividual studies to propose HASTE MRI as an alternative to chest x-ray in clinical practice."
View the group's full e-poster via the ESR website. Also, the authors have written up their findings in an article that is currently under revision for the British Journal of Radiology.