It remains to be seen whether the combination of MRI and PET will overtake the more established PET/CT, but specialists at King's College London (KCL) see the emerging hybrid imaging system as a powerful new tool in evaluating disease. They think the coupling of the two techniques could be part of a "paradigm shift" in cancer imaging, and in the future it may play a central role in diagnosing and treating neurological and cardiac diseases.
"It remains unclear how important PET/MRI will be as a clinical diagnostic tool," said Dr. Gary Cook, professor of clinical PET imaging and head of cancer imaging at KCL. "However, the evidence is slowly accumulating that in some clinical applications it gives better diagnostic accuracy than PET/CT or MRI alone."
Cook and his colleagues point to other advantages over PET/CT for patients, including a significant reduction in radiation dose and the convenience of a single appointment to replace the need for separate MR and PET/CT scans. Long-term, the hybrid examination is also seen as a possible cost-saving counterweight to the higher machinery costs.
The combination of advantages bodes well for a gradual shift from PET/CT to PET/MRI in the diagnosis and treatment of prostate, brain and gynecological tumors, according to Cook, who is based at the joint KCL and Guy's and St. Thomas' Hospital PET Centre, which had its formal opening in September 2014 in London.
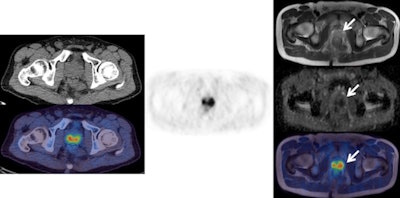
![Left: F-18 choline PET/CT (CT top and fused PET/CT bottom). Center: F-18 choline PET. Right: MRI (from top to bottom: T1, b900 diffusion-weighted image [DWI], apparent diffusion coefficient [ADC] map, fused PET/T1 MRI). These images show an enlarged choline-avid left pelvic lymph node in a man with high-risk Gleason 4+5 prostate cancer. This is clearly seen (arrow) on the PET/CT images, as well as on all the MRI sequences (high signal on b900 and restricted diffusion on ADC map). There is a small equivocal focus of uptake on the PET scan in the right side of the pelvis (arrow head), but it is difficult to confirm this is a lymph node on the CT and fused PET/CT images. The MRI sequences confirm a small lymph node with high signal on b900 DWI and restricted diffusion on ADC map (arrowhead). This case shows how the superior tissue contrast and anatomical resolution of MRI sequences allow a better definition of the cause of the right-sided pelvic PET activity and a much more confident diagnosis of right as well as left lymph node involvement. All images courtesy of Dr. Gary Cook.](https://img.auntminnieeurope.com/files/base/smg/all/image/2016/03/ame.2016_03_04_16_05_50_348_2016_03_05_ECR_Today_PET-MRI1.png?auto=format%2Ccompress&fit=max&q=70&w=400) Left: F-18 choline PET/CT (CT top and fused PET/CT bottom). Center: F-18 choline PET. Right: MRI (from top to bottom: T1, b900 diffusion-weighted image [DWI], apparent diffusion coefficient [ADC] map, fused PET/T1 MRI). These images show an enlarged choline-avid left pelvic lymph node in a man with high-risk Gleason 4+5 prostate cancer. This is clearly seen (arrow) on the PET/CT images, as well as on all the MRI sequences (high signal on b900 and restricted diffusion on ADC map). There is a small equivocal focus of uptake on the PET scan in the right side of the pelvis (arrow head), but it is difficult to confirm this is a lymph node on the CT and fused PET/CT images. The MRI sequences confirm a small lymph node with high signal on b900 DWI and restricted diffusion on ADC map (arrowhead). This case shows how the superior tissue contrast and anatomical resolution of MRI sequences allow a better definition of the cause of the right-sided pelvic PET activity and a much more confident diagnosis of right as well as left lymph node involvement. All images courtesy of Dr. Gary Cook.
Left: F-18 choline PET/CT (CT top and fused PET/CT bottom). Center: F-18 choline PET. Right: MRI (from top to bottom: T1, b900 diffusion-weighted image [DWI], apparent diffusion coefficient [ADC] map, fused PET/T1 MRI). These images show an enlarged choline-avid left pelvic lymph node in a man with high-risk Gleason 4+5 prostate cancer. This is clearly seen (arrow) on the PET/CT images, as well as on all the MRI sequences (high signal on b900 and restricted diffusion on ADC map). There is a small equivocal focus of uptake on the PET scan in the right side of the pelvis (arrow head), but it is difficult to confirm this is a lymph node on the CT and fused PET/CT images. The MRI sequences confirm a small lymph node with high signal on b900 DWI and restricted diffusion on ADC map (arrowhead). This case shows how the superior tissue contrast and anatomical resolution of MRI sequences allow a better definition of the cause of the right-sided pelvic PET activity and a much more confident diagnosis of right as well as left lymph node involvement. All images courtesy of Dr. Gary Cook."There may well be some new indications that are currently not routine with PET/CT that become adopted by PET/MRI," he explained, adding that these are likely to include novel tracers such as gallium-68 (68Ga) tracer, binding to prostate-specific membrane antigen (PSMA), as well as more conventional ones like F-18 fluorodeoxyglucose (F-18 FDG). "With regards to research, there is a great opportunity to exploit the synergistic potential of having molecular, functional, and anatomical data acquired simultaneously, especially for biological processes that may vary over time and where both PET and MRI signals can contribute, e.g., tumor hypoxia."
At today's session, ECR delegates will learn that the fusion of PET and MRI can produce an arsenal of simultaneous data for diagnosing and treating certain cancers. Yet for all its potential, PET/MRI is relatively untested in clinical settings and several challenges loom: high machinery costs, problems with artifacts, an absence of guidelines, and turf battles between nuclear medicine and radiology.
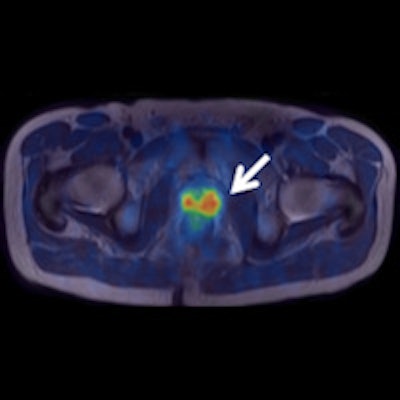
 Left: F-18 choline PET/CT (CT top and fused PET/CT bottom). Center: F-18 choline PET. Right: MRI (from top to bottom: T2, ADC map, fused PET/T2 MRI). The images clearly show abnormal choline activity in a large prostate cancer. However, the CT image does not allow any anatomical definition of the local extent of the tumor. The higher tissue contrast on the T2 MRI allows better definition (arrow) of the organ confined cancer, correlating with choline uptake on the fused PET/T2 MRI scan, and confirms restricted diffusion on the ADC map.
Left: F-18 choline PET/CT (CT top and fused PET/CT bottom). Center: F-18 choline PET. Right: MRI (from top to bottom: T2, ADC map, fused PET/T2 MRI). The images clearly show abnormal choline activity in a large prostate cancer. However, the CT image does not allow any anatomical definition of the local extent of the tumor. The higher tissue contrast on the T2 MRI allows better definition (arrow) of the organ confined cancer, correlating with choline uptake on the fused PET/T2 MRI scan, and confirms restricted diffusion on the ADC map.Beyond oncology, PET/MRI holds considerable promise in the diagnosis and care of neurological and cardiac patients, providing key data on what is taking place within organs and clues on whether therapies are working.
Hybrid PET/MRI technology is still a recent development, coming a decade after PET/CT systems hit the market in 2001. PET/CT revolutionized the ability to get a hybrid reading of both the molecular information provided by PET and the anatomical and morphological details offered through CT, using complementary data superior to what could be provided by fusing information from separate procedures. Results so far show the marriage of PET and MRI produces more quantitative data on the density and profusion of tumors.
Cook's colleague at the PET Centre, Dr. Vicky Goh, believes that PET/MRI represents a breakthrough, giving physicians the possibility to exploit the contrasts and resolution of an MRI with the molecular imaging powers of PET. The resulting comprehensive evaluation can be used to tailor care to an individual patient's needs.
"This is where we are seeing a paradigm shift" in patient care, said Goh, who is chair of clinical cancer imaging at KCL. "Gone are the days of simple size measurements, seeing whether a cancer is growing or shrinking, to evaluate if a treatment's working or not working. We now have a powerful imaging tool to assess cancer biology."
MRI provides better soft-tissue information, while PET provides the physiological data that can be particularly important in managing cancers such as in the prostate and the brain. PET/CT cannot provide such detail, she noted.
Yet Goh acknowledges that PET/MRI is still in a honeymoon period and there are drawbacks to PET/MRI for clinical use, at least at this juncture. For instance, there is a need to improve software to reduce artifacts and other distortions. There are also issues of affordability: A PET/MR system costs up to 5.5 million euros, more than double the price of a PET/CT scanner. Manufacturers are already addressing these deficiencies, however.
"A great deal of work is being carried out on methods to reduce artifacts and quantitative inaccuracies, and I am confident that most of the major problems will be overcome relatively quickly," Cook said.
Meanwhile, Goh dismisses criticism that PET is a very expensive research tool, or a very expensive toy. She points out that the hybrid system can save staff time, money, and patient stress by replacing two or more scans with a single operation.
KCL has also taken steps to train across disciplines to encourage the development of PET/MRI and improve the professional skills of physicians and technologists. This has helped ease some of the interdisciplinary conflicts that also emerged in the early development of PET/CT.
"Certainly it has been a learning experience for us, bringing together our nuclear medicine colleagues and our radiology colleagues and that may be easier in some places than others," she pointed out. "Where you are really seeing the adopters of PET/MR is where they have a good relationship."
Originally published in ECR Today on 5 March 2016.
Copyright © 2016 European Society of Radiology



















