How can medical imaging adopt artificial intelligence (AI) swiftly and effectively? Which factors tend to cause implementation delays? New research involving seven Dutch radiology departments has tried to provide answers to these burning questions.
Master's candidate Lea Strohm, from Utrecht University's Innovation Studies Group at the Copernicus Institute of Sustainable Development, sought to understand how the AI adoption process could best be organized. She collected data via document analysis and 24 semistructured interviews that lasted between 20 and 80 minutes and took place from January to June 2019. She conducted the interviews in English with a radiologist, technical staff, innovation managers, and members of other relevant organizations in the Dutch health system.
 Lea Strohm.
Lea Strohm."The underlying idea was that AI in radiology is overhyped," Strohm told AuntMinnieEurope.com. "There is a lot of research done on developing algorithms for specific applications, but barely any evidence of how the process of implementing these tools in clinical practice plays out. This was the knowledge gap I wanted to fill."
The research had two aims: to identify which factors facilitate and hinder the successful implementation of AI applications in radiology departments, and to specify how the hindering factors could be overcome. She then identified and adapted concepts arising from the interviews that could aid successful implementation of AI-based applications in clinical radiology in the Netherlands.
Facilitators and barriers
Strohm identified the following facilitating factors for the implementation of AI applications:
- Increased workloads and costs generate an openness toward any innovative technology that promises efficiency gains.
- AI promises added value in radiology.
- Openness toward new technology results in adoption of hospital-wide or radiology-specific innovation strategies, which include the use of AI.
She noted that successful implementation processes may be initiated and pushed forward by a "local champion," who is often a radiologist with a keen interest in development and a strong grasp of the technical aspects of AI applications. These individuals convince the other radiologists (direct adopters) and the referring clinicians (indirect adopters) of AI's benefits.
Implementing the applications without significant changes to routines also facilitates adoption as does integrating the applications as smoothly as possible into existing IT systems, such as PACS. Finally, the Radiological Society of the Netherlands (NVvR) is becoming increasingly active, providing a platform for knowledge exchange among its members, and this also promotes AI take-up, she noted.
Conversely, hindering factors include perceived inconsistent technical performance of most AI applications, and a lack of understanding of their technological aspects -- in turn causing doubt about quality and safety. Interviewees also considered the added value of AI applications for clinical radiology practice remains uncertain at present, due to a lack of scientific studies.
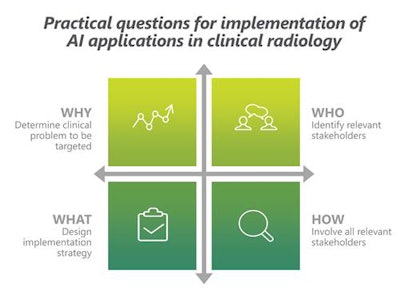 AI decision-makers need to ask themselves specific questions to ease implementation delays, as shown in these two charts. Images courtesy of Lea Strohm.
AI decision-makers need to ask themselves specific questions to ease implementation delays, as shown in these two charts. Images courtesy of Lea Strohm.Other negative factors include insufficient acceptance and trust of AI applications by radiologists and referring clinicians, while perceived changes to professional identity and professional responsibilities also have an impact on acceptance.
The interviews further revealed that another hurdle to adoption is the implementation processes of AI applications can be perceived as unstructured, not clearly establishing the clinical benefits to be achieved. Such processes fail to involve all relevant stakeholders, and do not specify how the application will be integrated in the clinical workflow or include implementation monitoring mechanisms.
Another barrier can be funding, due to the lack of clear evidence on AI's added value. Finally, changes in legislation on the use of personal data and medical devices, as well as questions of responsibility lead to legal uncertainties and make radiologists and hospitals uneasy.
Pointers for success
Strohm identified the following points that hospitals should consider ahead of implementing AI applications:
- Identify "local champions," particularly radiologists who are proactive in driving implementation projects.
- Implement inclusive decision-making processes: radiologists and referring clinicians (e.g., oncologists for oncological AI applications) should be part of specific purchasing decisions.
- Install monitoring mechanisms to monitor implementation and make sure AI applications are being used as planned.
"In one hospital, an AI application was implemented as part of a larger hospital-wide AI strategy decided by hospital management. This hospital also experienced relatively strong opposition to using AI-based applications from some radiologists," she said. "In hospitals where adoption decisions were taken in a more collaborative way, with the entire group of radiologists, opposition tended to be less strong."
While a collaborative decision process concerning AI technology can help raise acceptance, Strohm stressed her results cannot show a direct causal link between decision form and reception of AI.
"More generally, my research shows that a complex interplay of many different factors -- at an individual, organizational, and the wider 'health system' level -- determines the success and failure of adoption," she noted.
Her dissertation, "The augmented radiologist: Challenges and opportunities for wide-scale implementation of AI-based applications in Dutch radiology departments," was submitted in August.