Screening mammography exams arranged from low to high breast density can boost radiologists' interpretation performance, suggest findings published on 8 October in Radiology.
Researchers led by doctoral candidates Jessie Gommers and Sarah Verboom from Radboud University Medical Center in Nijmegen, the Netherlands, found slight improvements in the batch reading performance of radiologists when exams were ordered this way, as well as reduced reading times.
“Although larger studies are needed to validate these findings, our results suggest that ordering screening mammograms for reading by increasing volumetric breast density may be feasible,” the study authors wrote.
There is a need to strategize around identifying cancer in complex mammographic backgrounds, high volumes of screening exams, and the low prevalence of breast cancers at screening, the researchers suggested. This idea stems from previous studies' findings that between 20% and 50% of interval and screen-detected breast cancers were visible on prior screening mammograms.
Visual adaptation can impact screening performance. For batch reading, this requires interpreting radiologists to adapt to the characteristics of the mammogram they are reading. This means that mammograms for interpretation need to be ordered so that images with characteristics promoting similar visual adaptation are grouped together.
Gommers, Verboom, and colleagues studied how the screening performance of radiologists during batch reading of screening mammograms could be improved when the exams are ordered according to characteristics that may promote visual adaptation and fixation times (that is, the time the reader spends on the image).
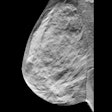
 Mammograms depict a 54-year-old woman with an invasive ductal carcinoma in the lateral upper quadrant of the left breast. The yellow dots represent eye fixations, and the red circle represents the lesion region. Image courtesy of the RSNA.
Mammograms depict a 54-year-old woman with an invasive ductal carcinoma in the lateral upper quadrant of the left breast. The yellow dots represent eye fixations, and the red circle represents the lesion region. Image courtesy of the RSNA.
The analysis included screening mammograms performed between 2016 and 2019 for 150 women with a median age of 55 years. Of the mammograms, 75 had breast cancer while the remaining 75 did not. The screening exams, each consisting of four mammograms, were interpreted by 13 radiologists in three distinct orders: randomly, by increasing volumetric breast density, and based on a self-supervised learning encoding. The researchers also employed an eye tracker to record eye movements by the radiologists.
Exams ordered by increasing breast density achieved the best marks of the three strategies, including having higher area under the curve (AUC) values and reduction in reading and fixation times.
| Results of batch reading ordering strategies | |||
|---|---|---|---|
| Measure | Random | Self-supervised learning | Volumetric breast density |
| AUC | 0.92 | 0.92 | 0.93 |
| Sensitivity | 81% | 80% | 81% |
| Specificity | 86% | 84% | 89% |
| Reading time | 27.9 seconds | 28.4 seconds | 24.3 seconds |
| Fixation time | 4.6 seconds | 4.6 seconds | 3.7 seconds |
| Fixation count | 52 | 54 | 47 |
| *Volumetric breast density strategy achieved statistical significance compared to random ordering for all measures except for sensitivity. Random ordering achieved statistical significance compared to self-supervised learning for fixation count and reading time. | |||
The study authors suggested that automated density algorithms could help organize screening program worklists and further improve the ability of radiologists to detect and characterize suspicious mammographic findings.
“However, future research should assess what other order criteria may further optimize radiologists’ screening performance,” they added. “If proven successful, future studies should also assess the effectiveness of these ordering strategies prospectively in actual screening settings.”
In an accompanying editorial, Dr. Lars Grimm, from Duke University in Durham, NC, wrote that the study’s results are promising.
“Although significant additional testing and refinement is needed, the findings represent a rare opportunity to improve breast radiologists’ interpretation performance and efficiency and are complementary to existing performance improvement measures, including batch reading and newer AI tools,” Grimm wrote.
The full study can be found here.